Measure Information Form
Version 2023A1
Measure Information Form
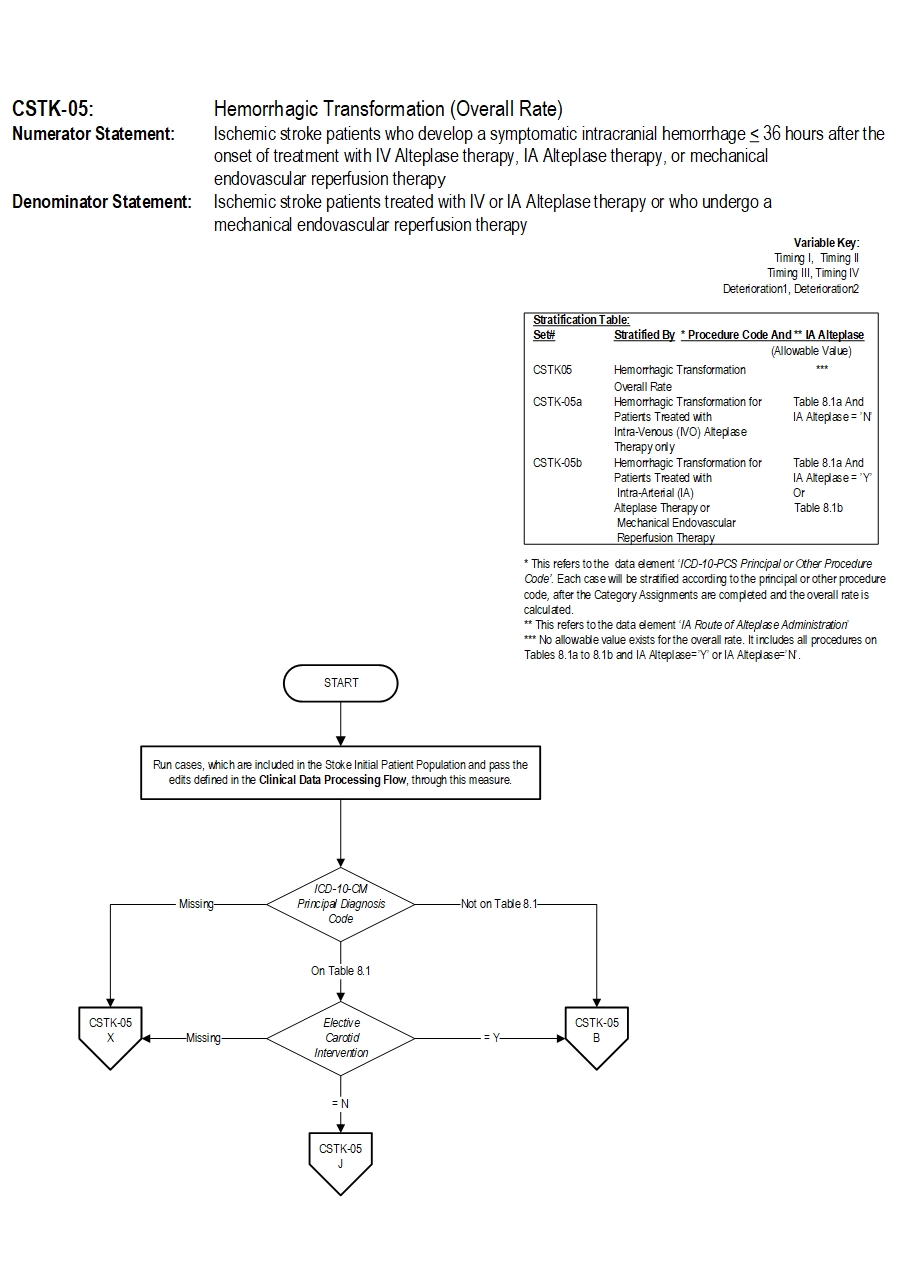
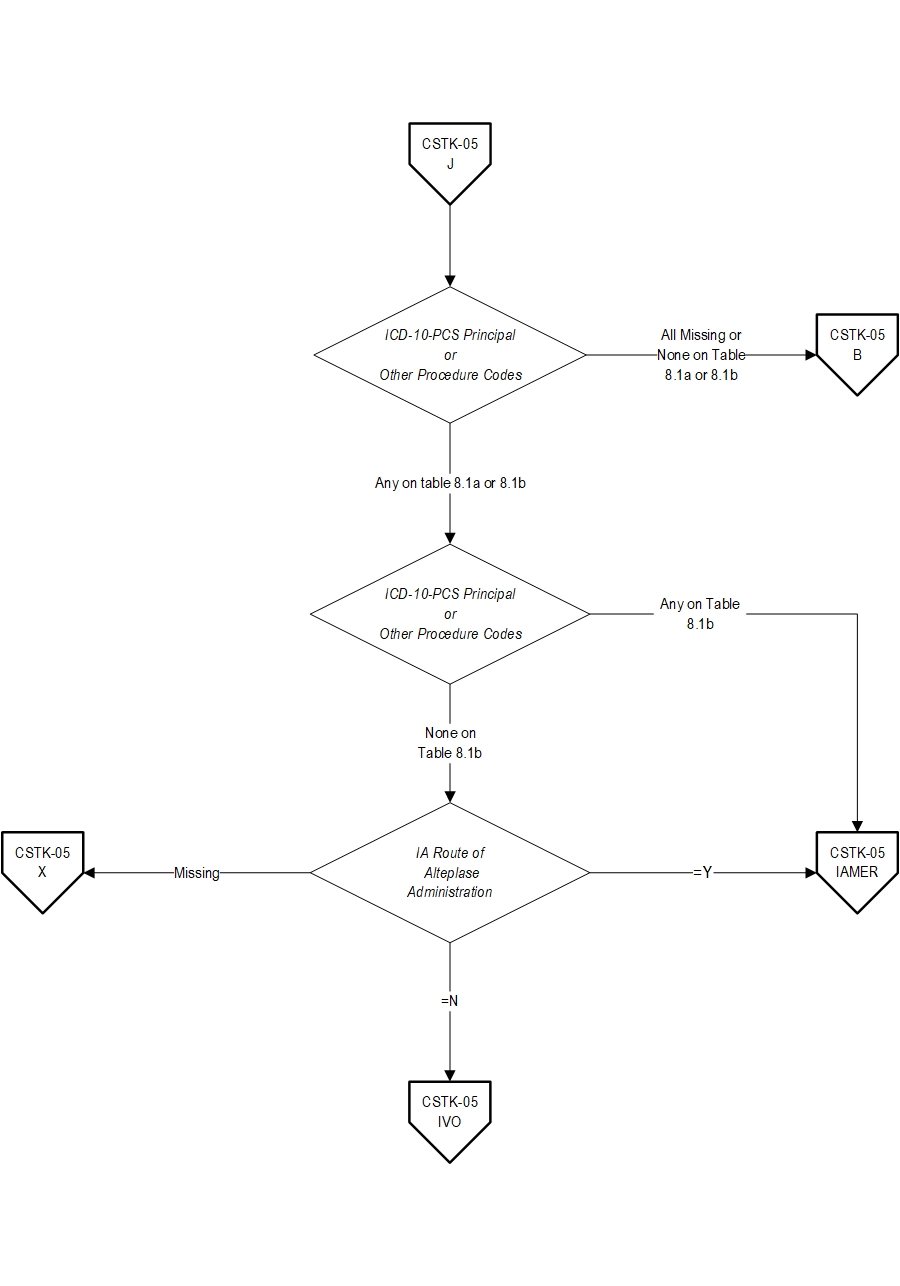
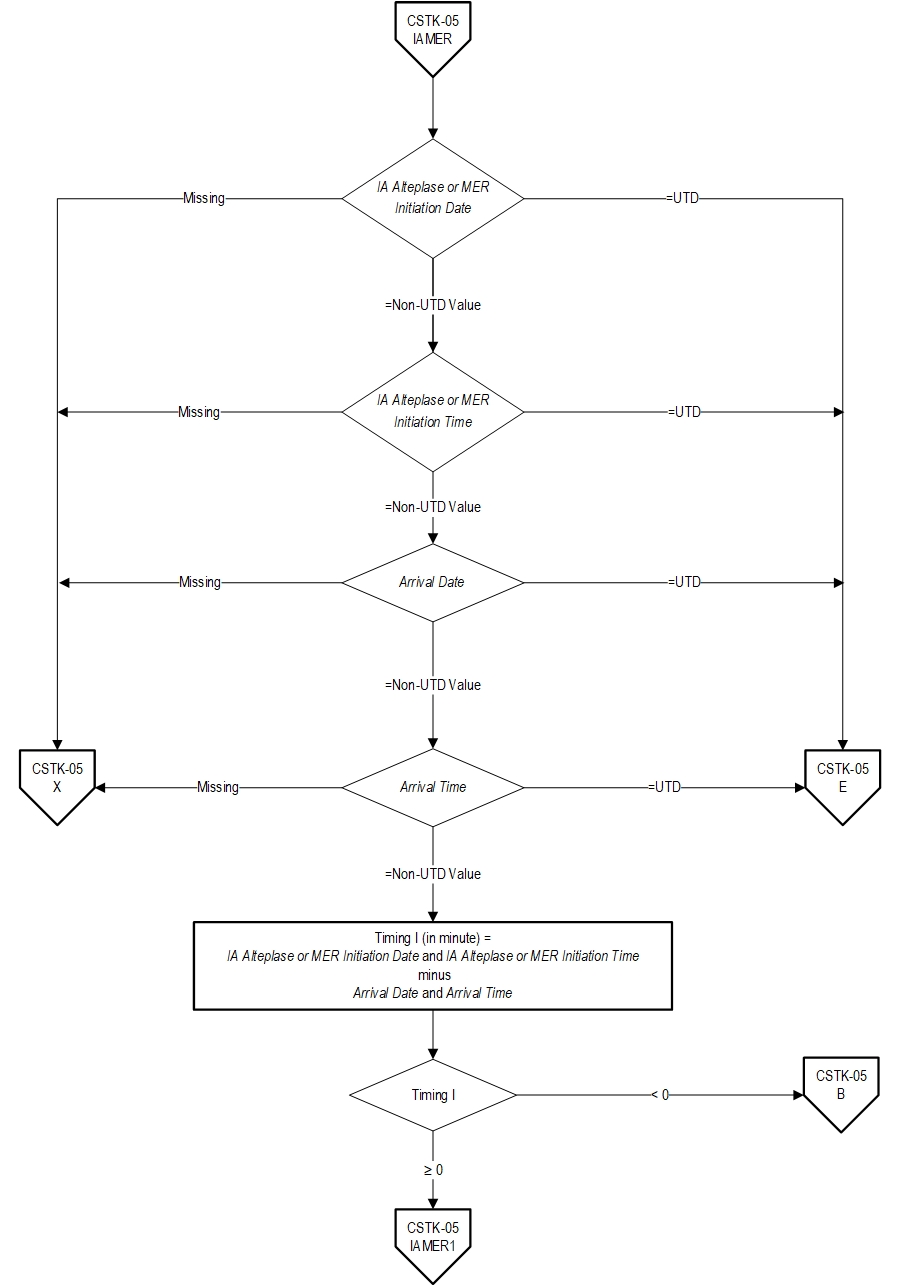
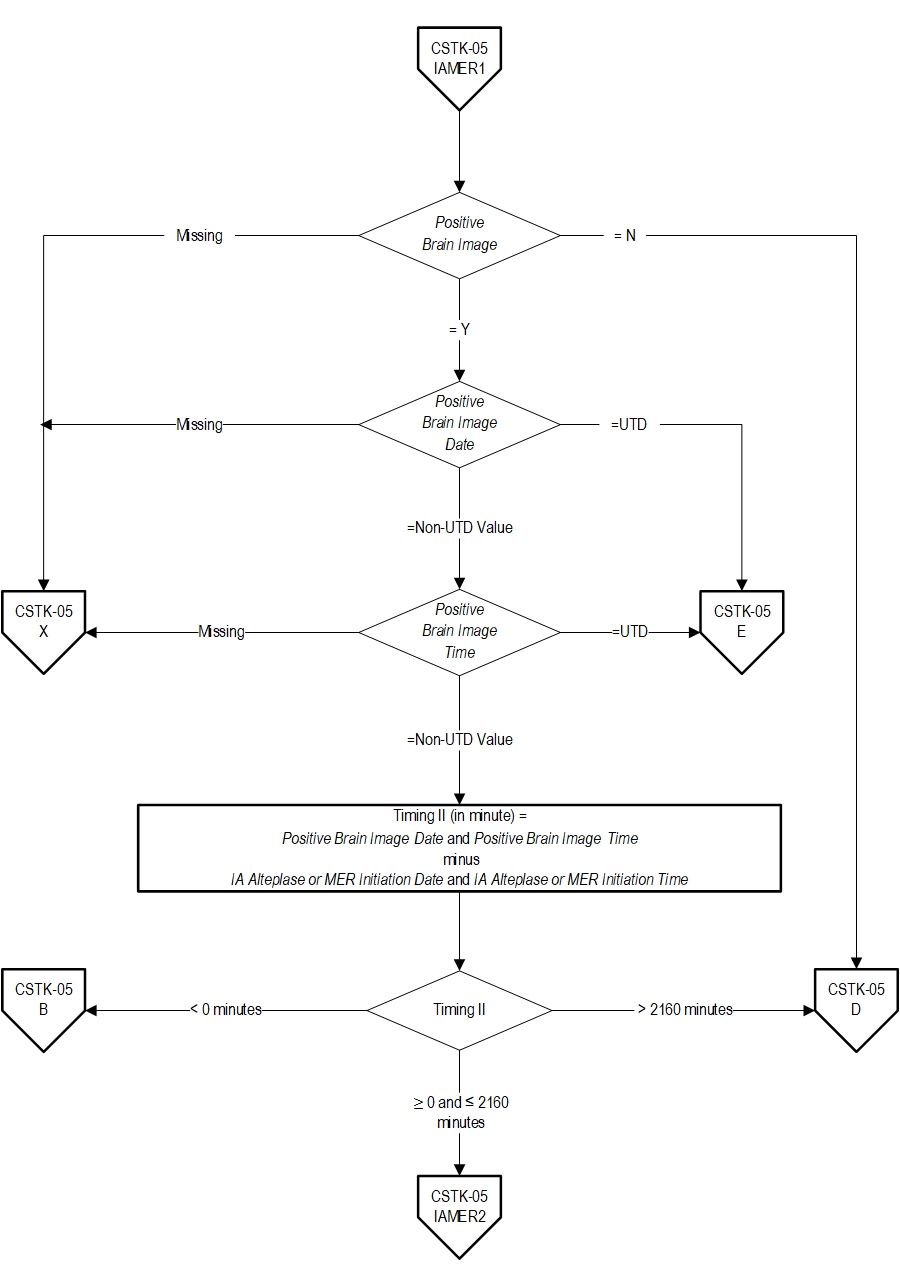
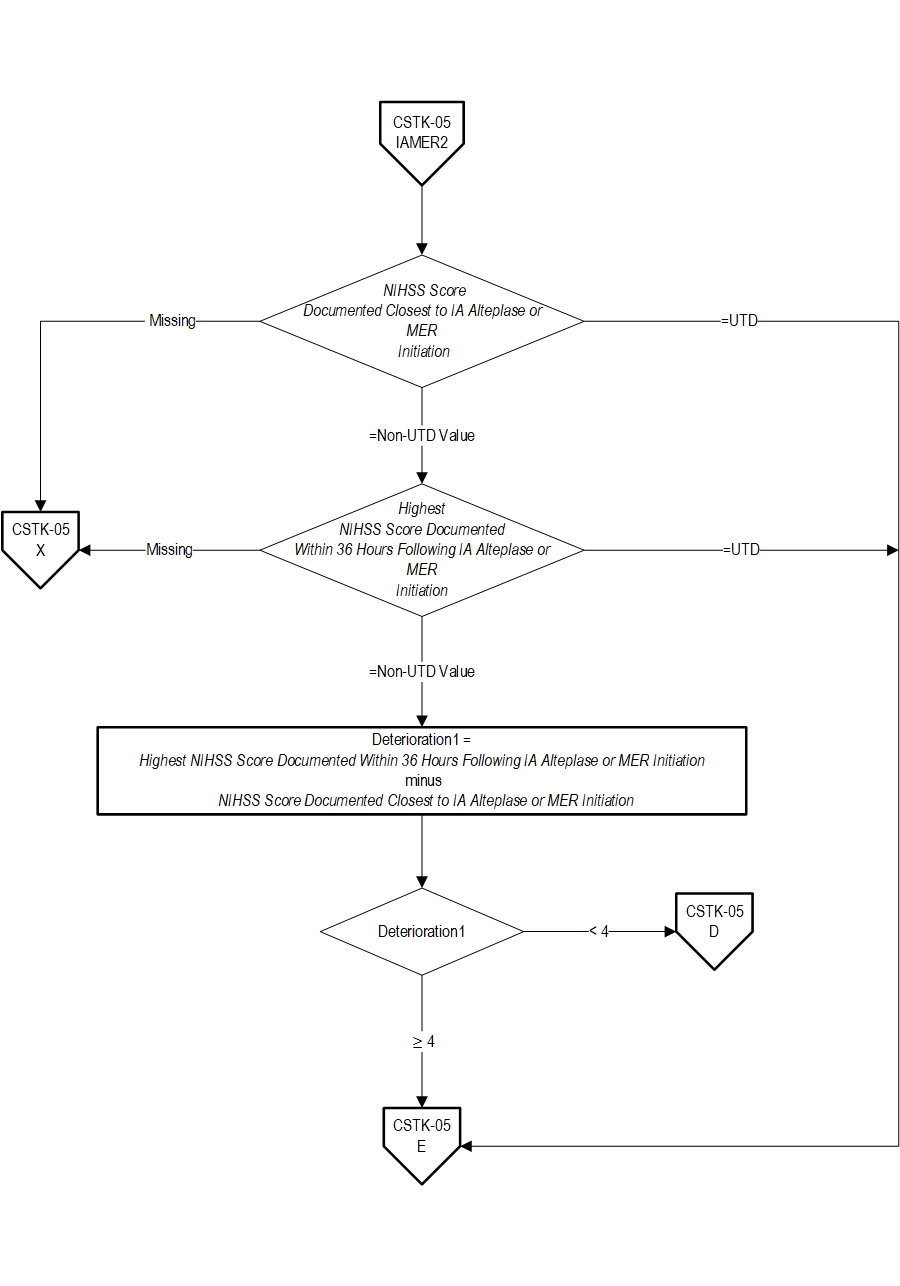
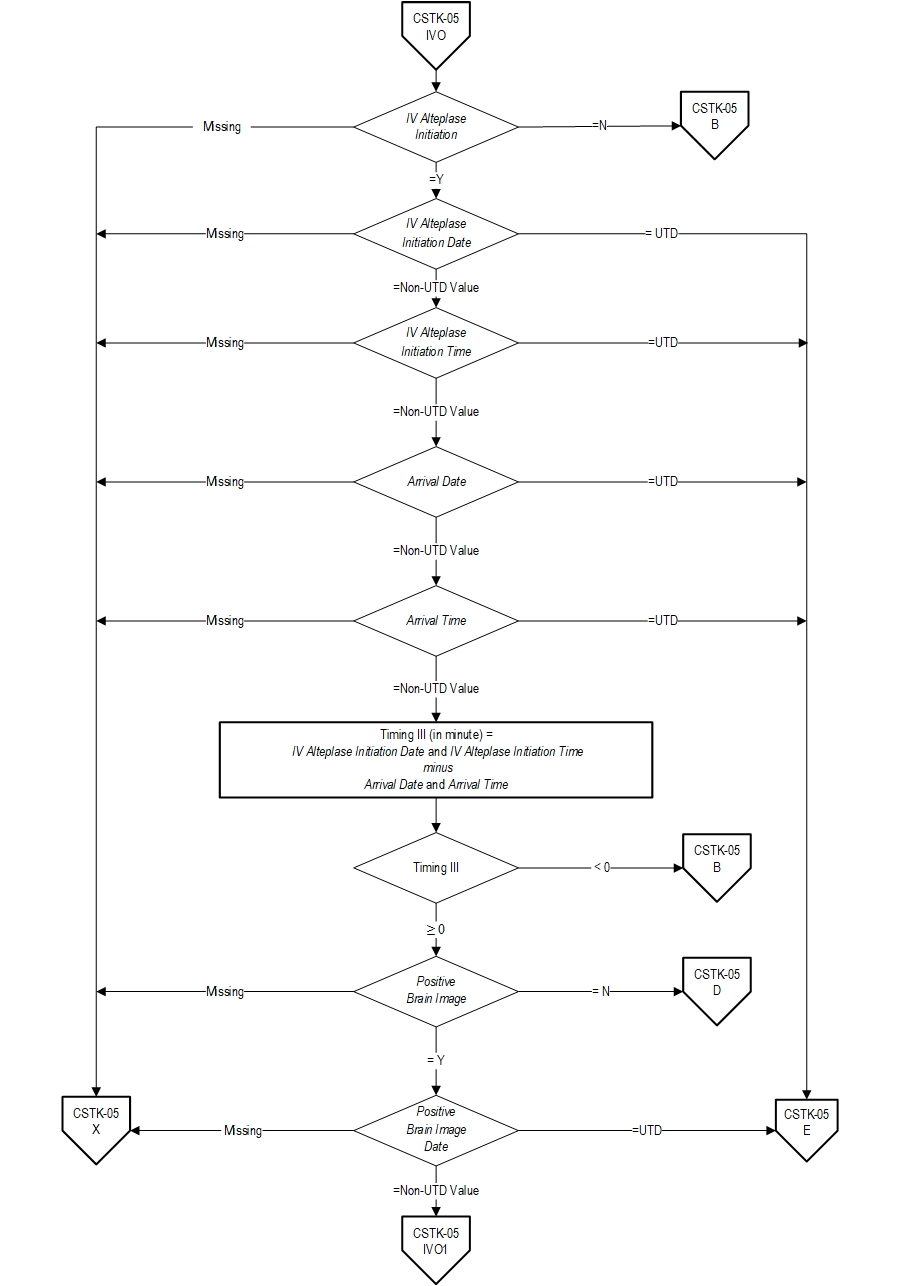
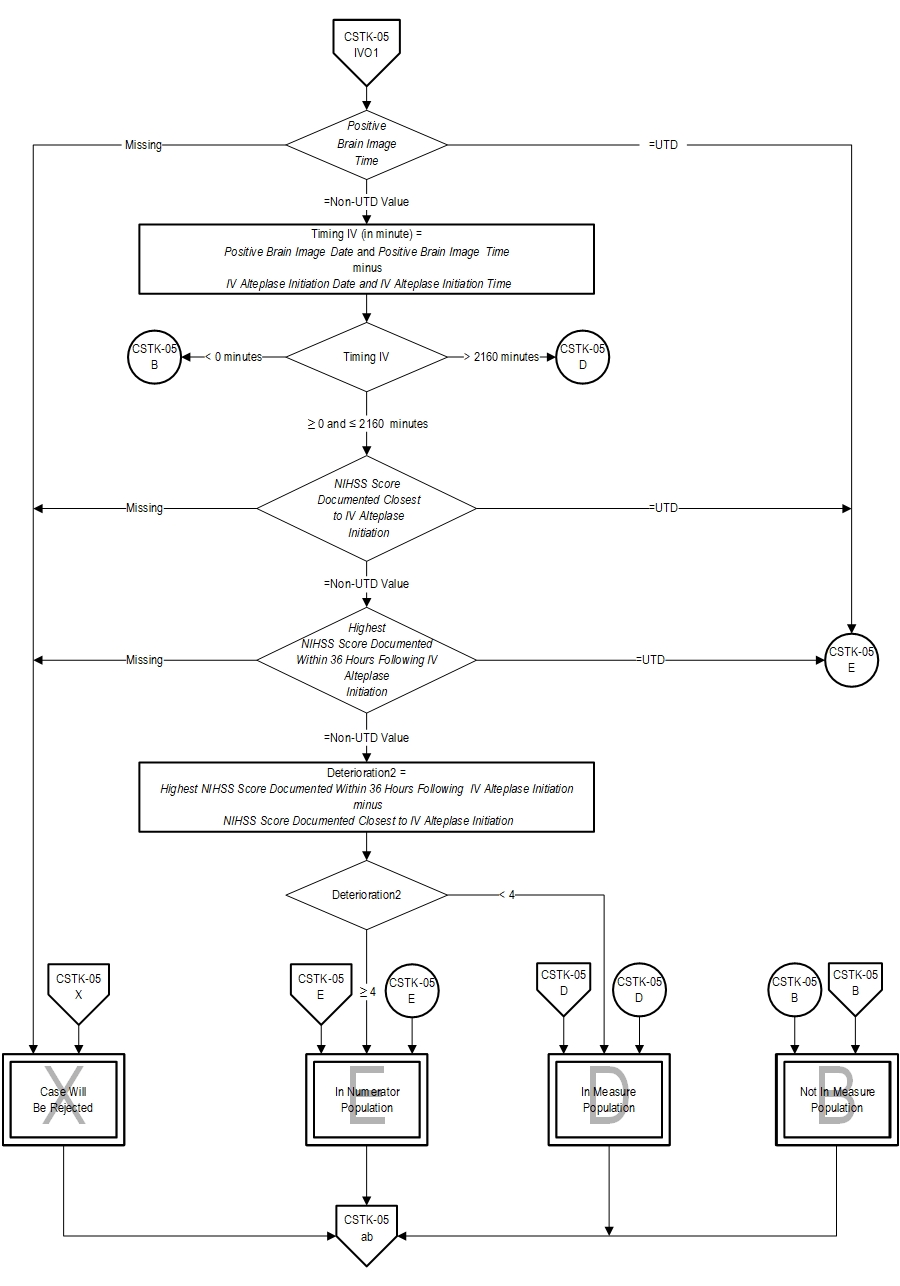
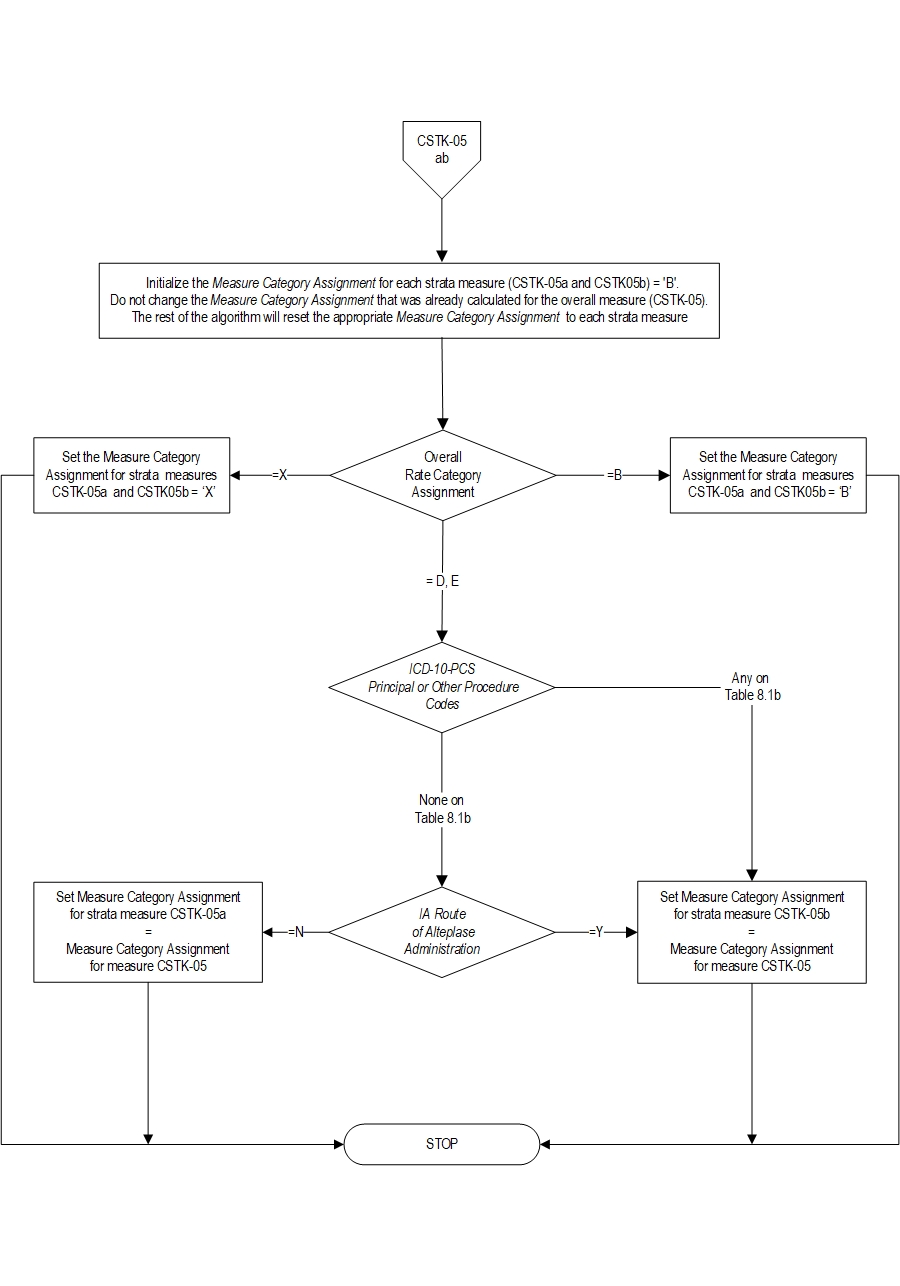
CSTK-05 Ischemic stroke patients who develop a symptomatic intracranial hemorrhage (i.e., clinical deterioration ≥ 4 point increase on NIHSS and brain image finding of parenchymal hematoma, or subarachnoid hemorrhage, or intraventricular hemorrhage) within (≤) 36 hours after the onset of treatment with intra-venous (IV) or intra-arterial (IA) alteplase therapy, or mechanical endovascular reperfusion procedure (i.e., mechanical endovascular thrombectomy with a clot retrieval device). CSTK-05a Ischemic stroke patients who develop a symptomatic intracranial hemorrhage (i.e., clinical deterioration ≥ 4 point increase on NIHSS and brain image finding of parenchymal hematoma, or subarachnoid hemorrhage, or intraventricular hemorrhage) within (≤) 36 hours after the onset of treatment with intra-venous (IV) alteplase therapy only. CSTK-05b Ischemic stroke patients who develop a symptomatic intracranial hemorrhage (i.e., clinical deterioration ≥ 4 point increase on NIHSS and brain image finding of parenchymal hematoma, or subarachnoid hemorrhage, or intraventricular hemorrhage) within (≤) 36 hours after the onset of treatment with IA alteplase therapy or mechanical endovascular reperfusion therapy (i.e., mechanical endovascular thrombectomy with a clot retrieval device).
The CSTK-05 measure is reported as an overall rate which includes ischemic stroke patients who develop a symptomatic hemorrhage after reperfusion therapy. CSTK-05a and CSTK-05b are subsets of the overall rate, and stratified by the type of therapy.
Rationale: Intravenous (IV) alteplase therapy for acute ischemic stroke was approved by the US Food and Drug Administration in 1996, following findings from the National Institute of Neurological Disorders and Stroke (NINDS) trial which demonstrated favorable outcomes in 31% to 50% of patients treated with recombinant tissue plasminogen activator (r-tPA), as compared to 20% to 38% of patients treated with placebo. Intra-arterial (IA) alteplase therapy has since been used to improve recanalization and clinical outcomes for select patients nonresponsive to IV therapy. Intracranial hemorrhage is the major risk of thrombolytic therapy with similar rates reported for both IV and IA routes. The NINDS trial found that 6.4% of patients treated with IV alteplase experienced symptomatic bleeding. Findings from the Prolyse in Acute Cerebral Thromboembolism (PROACT II) study found the intracranial hemorrhage with neurological deterioration within 24 hours occurred in 10% of patients treated with IA recombinant prourokinase. In addition to these agents, other available thrombolytic drugs include: streptokinase, p-anisoylated lys-plasminogen-streptokinase activator, and urokinase.Endovascular reperfusion therapy in acute ischemic stroke comprises a number of pharmacological and mechanical procedures. Mechanical endovascular thrombectomy is a treatment option for patients with large vessel occlusions in whom pharmacological thrombolysis is contraindicated or might be ineffective. For eligible patients, initiation of EVT (e.g., groin puncture) within 6 hours of stroke symptom onset using a stent retriever is preferred (Powers WJ, et. al., 2015). The use of mechanical thrombectomy devices other than stent retrievers as first-line devices for mechanical thrombectomy may be reasonable in some circumstances (Powers WJ, et. al., 2018). Mechanical endovascular thrombectomy devices are intended to improve tissue rescue and diminish reperfusion hemorrhage while broadening the population eligible for therapy. These devices may be used alone or in conjunction with chemical thrombolysis (i.e., IV or IA alteplase).
Type Of Measure: Outcome Improvement Noted As: Decrease in the rateCSTK-05 Ischemic stroke patients who develop a symptomatic intracranial hemorrhage ≤ 36 hours after the onset of treatment with IV alteplase therapy, or IA alteplase therapy, or mechanical endovascular reperfusion therapy CSTK-05a Ischemic stroke patients who develop a symptomatic intracranial hemorrhage ≤ 36 hours after the onset of treatment with IV alteplase therapy only (IVO) CSTK-05b Ischemic stroke patients who develop a symptomatic intracranial hemorrhage ≤ 36 hours after the onset of treatment with IA alteplase therapy or mechanical endovascular reperfusion therapy
Included Populations: As above Excluded Populations: None Data Elements:Data Elements By Measure
- Arrival Date
- Arrival Time
- Highest NIHSS Score Documented Within 36 Hours Following IA Alteplase or MER Initiation
- Highest NIHSS Score Documented Within 36 Hours Following IV Alteplase Initiation
- IA Alteplase or MER Initiation Date
- IA Alteplase or MER Initiation Time
- IA Route of Alteplase Administration
- IV Alteplase Initiation
- IV Alteplase Initiation Date
- IV Alteplase Initiation Time
- NIHSS Score Documented Closest to IA Alteplase or MER Initiation
- NIHSS Score Documented Closest to IV Alteplase Initiation
- Positive Brain Image
- Positive Brain Image Date
- Positive Brain Image Time
| CSTK-05 | CSTK-05a | CSTK-05b |
|---|---|---|
| Arrival Date | Arrival Date | Arrival Date |
| Arrival Time | Arrival Time | Arrival Time |
| Highest NIHSS Score Documented Within 36 Hours Following IA Alteplase or MER Initiation | Highest NIHSS Score Documented Within 36 Hours Following IV Alteplase Initiation | Highest NIHSS Score Documented Within 36 Hours Following IA Alteplase or MER Initiation |
| Highest NIHSS Score Documented Within 36 Hours Following IV Alteplase Initiation | IV Alteplase Initiation | IA Route of Alteplase Administration |
| IA Route of Alteplase Administration | IV Alteplase Initiation Date | IA Alteplase or MER Initiation Date |
| IA Alteplase or MER Initiation Date | IV Alteplase Initiation Time | IA Alteplase or MER Initiation Time |
| IA Alteplase or MER Initiation Time | NIHSS Score Documented Closest to IV Alteplase Initiation | NIHSS Score Documented Closest to IA Alteplase or MER Initiation |
| IV Alteplase Initiation | Positive Brain Image | Positive Brain Image |
| IV Alteplase Initiation Date | Positive Brain Date | Positive Brain Image Date |
| IV Alteplase Initiation Time | Positive Brain Image Time | Positive Brain Image Time |
| NIHSS Score Documented Closest to IA Alteplase or MER Initiation | ||
| NIHSS Score Documented Closest to IV Alteplase Initiation | ||
| Positive Brain Image | ||
| Positive Brain Image Date | ||
| Positive Brain Image Time |
Included Populations:Excluded Populations:
- Discharges with ICD-10-CM Principal Diagnosis Code for ischemic stroke as defined in Appendix A, Table 8.1 for ICD-10 codes,
AND- Patients with documented thrombolytic (IV or IA alteplase) therapy (ICD-10-PCS Principal or Other Procedure Codes as defined in Appendix A, Table 8.1a for ICD-10 codes ),
OR- Patients with documented Mechanical Endovascular Reperfusion Therapy (ICD-10-PCS Principal or Other Procedure Codes as defined in Appendix A, Table 8.1b for ICD-10 codes)
Data Elements:
- Patients less than 18 years of age
- Patients who have a Length of Stay > 120 days
- Patients admitted for Elective Carotid Intervention
- Patients transferred to this hospital following treatment with IV alteplase therapy or IA alteplase therapy or mechanical endovascular reperfusion therapy initiated prior to arrival at this hospital
- Patients who hemorrhage prior to the onset of treatment with IV alteplase or IA thrombolytic alteplase or mechanical endovascular reperfusion therapy
- Adams HP Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, Grubb RL, Higashida RT, Jauch EC, Kidwell C, Lyden PD, Morgenstern LB, Qureshi AI, Rosenwasser RH, Scott PA, Wijdicks E. Guidelines for the Early Management of Adults with Ischemic Stroke: A Guideline From the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups. Stroke. 2007;38:1664-1666.
- Adams HP Jr, Brott TG, Furlan AJ, Gomez, CR, Grotta J, Helgason CM, Kwiatkowski T, Lyden PD, Marler JR, Torner J, Feinberg W, Mayberg M, Thies W. Guidelines for thrombolytic therapy for acute stroke: a supplement to the guidleines for the management of patients with acute ischemic stroke. Circulation.1996;94;1167-1174.
- Broderick JP, Palesch YY, Demchuk AM, et al. Endovascular treatment after intravenous t-PA versus t-PA alone for stroke. NEJM. 2013;368:893-903.
- Campbell BCV, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et. al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. NEJM. 2015 Mar;372(11): 1009-17.
- Ciccone A, Valvassori, Nichelatti M, et. al. Endovascular treatment for acute ischemic stroke. NEJM. 2013;368:904-913.
- delZoppo GJ, Higashida RT, Furlan AJ, Pessin MS, Gent M, Driscoll RM, and the PROACT Investigators. The Prolyse in Acute Cerebral Thromboembolism Trial (PROACT): results of 6 mg dose tier. Stroke. 1996;27:164.
- delZoppo GJ, Higashida RT, Furlan AJ. The case for a phase III trial of cerebral intraarterial fibrinolysis. AJNR Am J Neuroradiol. 1994; 15:1217-1222.
- Demchuk AM, Goyal M, Monon BK, Eesa M, Ryckborst KJ, Kamal N, et. al. Endovascular treatment for Small Core and Anterior circulation Proximal occlusion with Emphasis on minimizing CT to recanalization times (ESCAPE) trial: methodology. Int J Stroke. 2015 Apr;10(3): 429-38.
- Donnen GA, Davis SM, Chambers BR, Gates PC, Hankey GJ, McNeil JJ, Rosen D, Stewart-Wynne EG, Tuck RR. Trials of streptokinase in severe acute ischaemic stroke. Lancet. 1995; 345: 578-579.
- Fibrinolytic Therapy Trialist's (FTT) Collaborative Group. Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomized trials of more than 1000 patients. Lancet. 1994;343:311-322.
- Hacke W, Kaste M, Fieschi C, Toni D, Lesaffre E, von Kummer R, Boysen G, Bluhmki E, Hoxter G, Mahagne MH, Hennerici M, for the ECASS Study Group. Intravenous thrmbolysis with recombinant tissue plasminogen activator for acute hemispheric stroke: the European Cooperative Acute Stroke Study. JAMA. 1995; 274: 1017-1025.
- Jauch EC, Saver JL, Adams HP Jr, Bruno A, Connors JJ, Demaerschalk BM, Khatri P, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:32-36.
- Kidwell CS, Jahan R, Gornbein J, et. al. A trial of imaging selection and endovascular treatment for ischemic stroke. NEJM. 2013;368:914-923.
- Koh JS, et al: Safety and efficacy of mechanical thrombectomy with Solitaire stent retrieval for acute ischemic stroke: a systematic review. Neurointervention. 2012;7:1-9.
- Leifer D, Bravata DM, Connors JJ III, Hinchey JA, Jauch EC, Johnston SC, Latchaw R, Likosky W, Ogilvy C, Qureshi AI, Summers D, Sung GY, Williams LS, Zorowitz R, on behalf of the American Heart Association Special Writing Group of the Stroke Council, Atherosclerotic Peripheral Vascular Disease Working Group and Council on Cardiovascular Surgery and Anesthesia, and Council on Cardiovascular Nursing. Metrics for measuring quality of care in comprehensive stroke centers: detailed follow-up to Brain Attack Coalition comprehensive stroke center recommendations: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:858.
- Levy DE, Brott TG, Haley EC Jr, Marler JR, Sheppard GL, Barsan W, Broderick JP. Factors related to intracranial hematoma formation in patients receiving tissue-type plasminogen activator for acute ischemic stroke. Stroke. 1994;25:291-297.
- Marder VJ, Sherry S. Thrombolytic therapy: current status. N Engl J Med. 1988;318:1512-1520.
- Menon BK, Saver JL, Prabhakaran S, Reeves M, Liang L, Olson DWM, Peterson ED, Hernandez AF, Fonarow GC, Schwamm LH, Smith EE. Risk score for intracranial hemorrhage in patients with acute ischemic stroke treated with intravenous tissue-type plasminogen activator. Stroke. 2012;43: 1-9.
- Multicenter Acute Stroke Trail-Italy (MAST-I) Group. Randomised controlled trial of streptokinase, aspirin, and combination of both in treatment of acute ischaemic stroke. Lancet. 1995;346:1509-1514.
- Nogueira RG, Lutsep HL, Gupta R, Jovin TG, Albers GW, Walker GA, Liebeskind DS, Smith WS, for the TREVO 2 Trialists. Trevo versus Merci retrievers for thrombectomy revascularization of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomized trial. Lancet. 2012;380:1231-1240.
- Powers WJ, Derdeyn CP, Biller J, Coffey CS, Jauch EC, Johnston KC, Johnston SC, Khalessi AA, Kidwell CS, Meschia JF, Ovbiagele B, Yavagal DR, on behalf of the American Heart Association Stroke Council. 2015 AHA/ASA focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46; 3021-3035.
- Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, et al; on behalf of the American Heart Association Stroke Council. 2018 Guidelines for the Early Management of Patients with Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2018 Jan;49:e18-e30.
- Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, et al. Guidelines for the Early Management of Patients with Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke. A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2019 Dec;50(12):e344-e418.
- Rubiera M, Ribo M, Pagola J, Coscojuela P, Rodrigues-Luna D, Maisterra O, Ibarra B, Piñeiro S, Meler P, Romero FJ, Alvarez-Sabin J, Molina CA. Bridging intravenous-intra-arterial rescue strategy increases recanalization and the likelihood of a good outcome in nonresponder intravenous tissue plasminogen activator-treated patients: a case-control study. Stroke. 2011 Apr;42(4):993-997.
- Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et. al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. NEJM. 2015 Apr: 1-11.
- Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, Clark W, Budzik R, Zaidat OO, for the SWIFT Trialists. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomized, parallel-group, non-inferiority trial. Lancet. 2012;380:1241-1249.
- Sims JR, Gharai R, Schaefer PW, Vangel M, Rosenthal ES, Lev MH, Schwamm LH. ABC/2 for rapid clinical estimate of infarct, perfusion, and mismatch volumes. Neurology. 2009;72:2104-2110.
- Sloan MA, Price TR, Petito CK, Randall AM, Solomon RE, Terrin ML, Gore J, Collen D, Kleiman N, Feit F, Babb J, Herman M, Roberts WC, Spoko G, Bovill E, Forman S, Knatterud GL, for the TIMI Investigators. Clinical Features and pathogenesis of intracerebral hemorrhage after rt-PA and heparin therapy for acute myocardial infarction: the TIMI II pilot and randomisezed clinical trial combined experience. Neurologoy. 1995;45:649-658.
- Smith WS, et al. Mechanical thrombectomy for acute ischemic stroke. Stroke. 2008;39:1205-1212.
- The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333:1581-1587.
- Turk AS, Frei D, Fiorella D, Mocco J, Baxter B, Siddiqui A, et. al. ADAPT FAST study: a direct aspiration first pass technique for acute stroke thrombectomy. J Neurointerv Surg. 2014 May;694): 260-4.
CPT® only copyright 2022 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association.
You, your employees and agents are authorized to use CPT® only as contained in The Joint Commission performance measures solely for your own personal use in directly participating in healthcare programs administered by The Joint Commission. You acknowledge that the American Medical Association (“AMA”) holds all copyright, trademark and other rights in CPT®.
Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CPT® for resale and/or license, transferring copies of CPT® to any party not bound by this Agreement, creating any modified or derivative work of CPT®, or making any commercial use of CPT®. License to use CPT® for any use not authorized herein must be obtained through the American Medical Association, Intellectual Property Services, AMA Plaza, 330 North Wabash Avenue, Suite 39300, Chicago, Illinois 60611-5885. Applications are available at the American Medical Association Web site, www.ama- assn.org/go/cpt.
U.S. Government Rights This product includes CPT® which is commercial technical data, which was developed exclusively at private expense by the American Medical Association, 330 North Wabash Avenue, Chicago, Illinois 60611. The American Medical Association does not agree to license CPT® to the Federal Government based on the license in FAR 52.227-14 (Data Rights - General) and DFARS 252.227-7015 (Technical Data - Commercial Items) or any other license provision. The American Medical Association reserves all rights to approve any license with any Federal agency.
Disclaimer of Warranties and Liabilities. CPT® is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to the implied warranties of merchantability and fitness for a particular purpose. Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT®, and the (AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this product is with The Joint Commission, and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this product.
This Agreement will terminate upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
Should the foregoing terms and conditions be acceptable to you, please indicate your agreement and acceptance by clicking below on the button labeled “accept”.