Measure Information Form
Version 2023B
Measure Information Form
As compared to other CB measures, what is different about NTSV CB rate (Primary CB in first births with term singleton pregnancies in head down position) is that there are clear cut quality improvement activities that can be done to address the differences. Main et al. (2012) found that over 60% of the variation among hospitals can be attributed to first birth labor induction rates and first birth early labor admission rates. The results showed if labor was forced when the cervix was not ready the outcomes were poorer. Rosenstein et al. (2021) also showed that labor and delivery guidelines can make a difference in labor outcomes. Many authors have shown that physician factors, rather than patient characteristics or obstetric diagnoses are the major driver for the difference in rates within a hospital (Berkowitz, et al.,1989; Goyert et al., 1989; Luthy et al., 2003, Symum et al., 2021). The dramatic variation in cesarean rates seen in all populations studied is striking. (Cesarean rates varied tenfold in US hospitals nationwide across hospitals, from 7.1 % to 69.9 % and there was a 15-fold variation among low-risk women, from 2.4% to 36.5% (Kozhimannil et al., 2013).
A reduction in the number of nulliparous patients with live term singleton newborns in vertex position (NTSV) delivering by cesarean birth will result in increased patient safety, a substantial decrease in maternal and neonatal morbidity and substantial savings in health care costs. Successful quality improvement efforts incorporate audit and feedback strategies combined with provider and nurse education, guidelines and peer review.
The measure will assist health care organizations (HCOs) to track nulliparous patients with live term singleton newborns in vertex position delivering by cesarean birth to reduce the occurrence. Nulliparous women have 4-6 times the cesarean birth rate than multiparous women thus the NTSV population is the largest driver of primary cesarean birth rate (Sakala et al., 2020). NTSV has a large variation among facilities, thus identifying an important population on which to focus quality improvement efforts.
In addition, a reduction in primary cesarean births will reduce the number of women having repeat cesarean births (almost 90% of mothers who have a primary cesarean birth will have subsequent cesarean birth (CDC, 2020)). Thus, improvement in the rates of cesarean birth for the first birth will reduce the morbidity of all future births and avoid all the controversies with trial of labor after cesarean/elective repeat cesareans.
Type Of Measure: Outcome Improvement Noted As: Within Optimal RangeIncluded Populations: ICD-10-PCS Principal Procedure Code or ICD-10-PCS Other Procedure Codes for cesarean birth as defined in Appendix A, Table 11.06 Cesarean Birth Excluded Populations: None Data Elements:Denominator Statement: Nulliparous patients delivered of a live term singleton newborn in vertex presentation
Included Populations:Excluded Populations:
- ICD-10-PCS Principal Procedure Code or ICD-10-PCS Other Procedure Codes for delivery as defined in Appendix A, Table 11.01.1 Delivery
- Nulliparous patients with ICD-10-CM Principal Diagnosis Code or ICD-10-CM Other Diagnosis Codes for outcome of delivery as defined in Appendix A, Table 11.08 Outcome of Delivery and with a delivery of a newborn with 37 weeks or more of gestation completed
Data Elements:
- ICD-10-CM Principal Diagnosis Code or ICD-10-CM Other Diagnosis Codes for multiple gestations and other presentations as defined in Appendix A, Table 11.09 Multiple Gestations and Other Presentations
- Less than 8 years of age
- Greater than or equal to 65 years of age
- Length of Stay >120 days
- Gestational Age < 37 weeks or UTD
- Agency for Healthcare Research and Quality. (2002). AHRQ Quality Indicators Guide to Inpatient Quality Indicators: Quality of Care in Hospitals Volume, Mortality, and Utilization. Revision 4 (December 22, 2004). AHRQ Pub. No. 02-RO204.
- American College of Obstetricians and Gynecologists. (2000). Task Force on Cesarean Delivery Rates. Evaluation of Cesarean Delivery. (Developed under the direction of the Task Force on Cesarean Delivery Rates, Roger K. Freeman, MD, Chair, Arnold W. Cohen, MD, Richard Depp III, MD, Fredric D. Frigoletto Jr, MD, Gary D.V. Hankins, MD, Ellice Lieberman, MD, DrPH, M. Kathryn Menard, MD, David A. Nagey, MD, Carol W. Saffold, MD, Lisa Sams, RNC, MSN and ACOG Staff: Stanley Zinberg, MD, MS, Debra A. Hawks, MPH, and Elizabeth Steele)
- Bailit, J.L., Garrett, J.M., Miller, W.C., McMahon, M.J., & Cefalo, R.C. (2002). Hospital primary cesarean delivery rates and the risk of poor neonatal outcomes. Am J Obstet Gynecol. 187(3):721-7.
- Bailit, J. & Garrett, J. (2003). Comparison of risk-adjustment methodologies. Am J Obstet Gynecol.102:45-51.
- Bailit, J.L., Love, T.E., & Dawson, N.V. (2006). Quality of obstetric care and risk-adjusted primary cesarean delivery rates. Am J Obstet Gynecol.194:402.
- Bailit, J.L. (2007). Measuring the quality of inpatient obstetrical care. Ob Gyn Sur. 62:207-213.
- Berkowitz, G.S., Fiarman, G.S., Mojica, M.A., et al. (1989). Effect of physician characteristics on the cesarean birth rate. Am J Obstet Gynecol. 161:146-9.
- Center for Disease Control (2020). Recent trends in vaginal birth after cesarean delivery: United States, 2016-2018. Retrieved from National Center for Health Statistics: https://www.cdc.gov/nchs/products/databriefs/db359.htm
- Cleary, R., Beard, R.W., Chapple, J., Coles, J., Griffin, M., & Joffe, M. (1996). The standard primipara as a basis for inter-unit comparisons of maternity care. Br J Obstet Gynecol. 103:223-9.
- DiGiuseppe, D.L., Aron, D.C., Payne, S.M., Snow, R.J., Dieker, L., & Rosenthal, G.E. (2001). Risk adjusting cesarean delivery rates: a comparison of hospital profiles based on medical record and birth certificate data. Health Serv Res.36:959-77.
- Goyert, G.L., Bottoms, F.S., Treadwell, M.C., et al. (1989). The physician factor in cesarean birth rates. N Engl J Med.320:706-9.
- Kozhimannil, K. B., Law, M. R., & Virnig, B. A. (2013). Cesarean delivery rates vary tenfold among US hospitals; reducing variation may address quality and cost issues. Health affairs (Project Hope), 32(3), 527–535. https://doi.org/10.1377/hlthaff.2012.1030
- Le Ray, C., Carayol, M., Zeitlin, J., Berat, G., & Goffinet, F. (2006). Level of perinatal care of the maternity unit and rate of cesarean in low-risk nulliparas. Am J Obstet Gynecol. 107:1269-77.
- Luthy, D.A., Malmgren, J.A., Zingheim, R.W., & Leininger, C.J. (2003). Physician contribution to a cesarean delivery risk model. Am J Obstet Gynecol.188:1579-85.
- Main E.K., Bloomfield, L., & Hunt, G. (2004). Development of a large-scale obstetric quality-improvement program that focused on the nulliparous patient at term. Am J Obstet Gynecol.190:1747-58.
- Main, E. K., Chang, S. C., Cape, V., Sakowski, C., Smith, H., & Vasher, J. (2019). Safety Assessment of a Large-Scale Improvement Collaborative to Reduce Nulliparous Cesarean Delivery Rates. Obstetrics and gynecology, 133(4), 613–623. https://doi.org/10.1097/AOG.0000000000003109
- Main, E.K., Moore, D., Farrell, B., Schimmel, L.D., Altman, R.J., Abrahams, C., et al., (2006). Is there a useful cesarean birth measure? Assessment of the nulliparous term singleton vertex cesarean birth rate as a tool for obstetric quality improvement. Am J Obstet Gynecol. 194:1644-51.
- Main, E. K., Morton, C. H., Melsop, K., Hopkins, D., Giuliani, G., & Gould, J. B. (2012). Creating a public agenda for maternity safety and quality in cesarean delivery. Obstetrics and gynecology, 120(5), 1194–1198. https://doi.org/10.1097/aog.0b013e31826fc13d
- Romano, P.S., Yasmeen, S., Schembri, M.E., Keyzer, J.M., & Gilbert, W.M. (2005). Coding of perineal lacerations and other complications of obstetric care in hospital discharge data. Am J Obstet Gynecol.106:717-25.
- Rosenstein, M. G., Chang, S. C., Sakowski, C., Markow, C., Teleki, S., Lang, L., Logan, J., Cape, V., & Main, E. K. (2021). Hospital Quality Improvement Interventions, Statewide Policy Initiatives, and Rates of Cesarean Delivery for Nulliparous, Term, Singleton, Vertex Births in California. JAMA, 325(16), 1631–1639. https://doi.org/10.1001/jama.2021.3816
- Sakala, C., Belanoff, C., & Declercq, E. R. (2020). Factors Associated with Unplanned Primary Cesarean Birth: Secondary Analysis of the Listening to Mothers in California Survey. BMC pregnancy and childbirth, 20(1), 462. https://doi.org/10.1186/s12884-020-03095-4
- Symum, H., & Zayas-Castro, J. L. (2021). A Multistate Decomposition Analysis of Cesarean Rate Variations, Associated Health Outcomes, and Financial Implications in the United States. American journal of perinatology, 10.1055/s-0041-1736538. Advance online publication. https://doi.org/10.1055/s-0041-1736538
- U.S. Department of Health and Human Services. (n.d.). Reduce cesarean births among low-risk women with no prior births-MICH-06. Retrieved from Healthy People 2030: https://health.gov/healthypeople/objectives-and-data/browse-objectives/pregnancy-and-childbirth/reduce-cesarean-births-among-low-risk-women-no-prior-births-mich-06
- Yasmeen, S., Romano, P.S., Schembri, M.E., Keyzer, J.M., & Gilbert, W.M. (2006). Accuracy of obstetric diagnoses and procedures in hospital discharge data. Am J Obstet Gynecol. 194:992-1001.
California Maternal Quality Care Collaborative
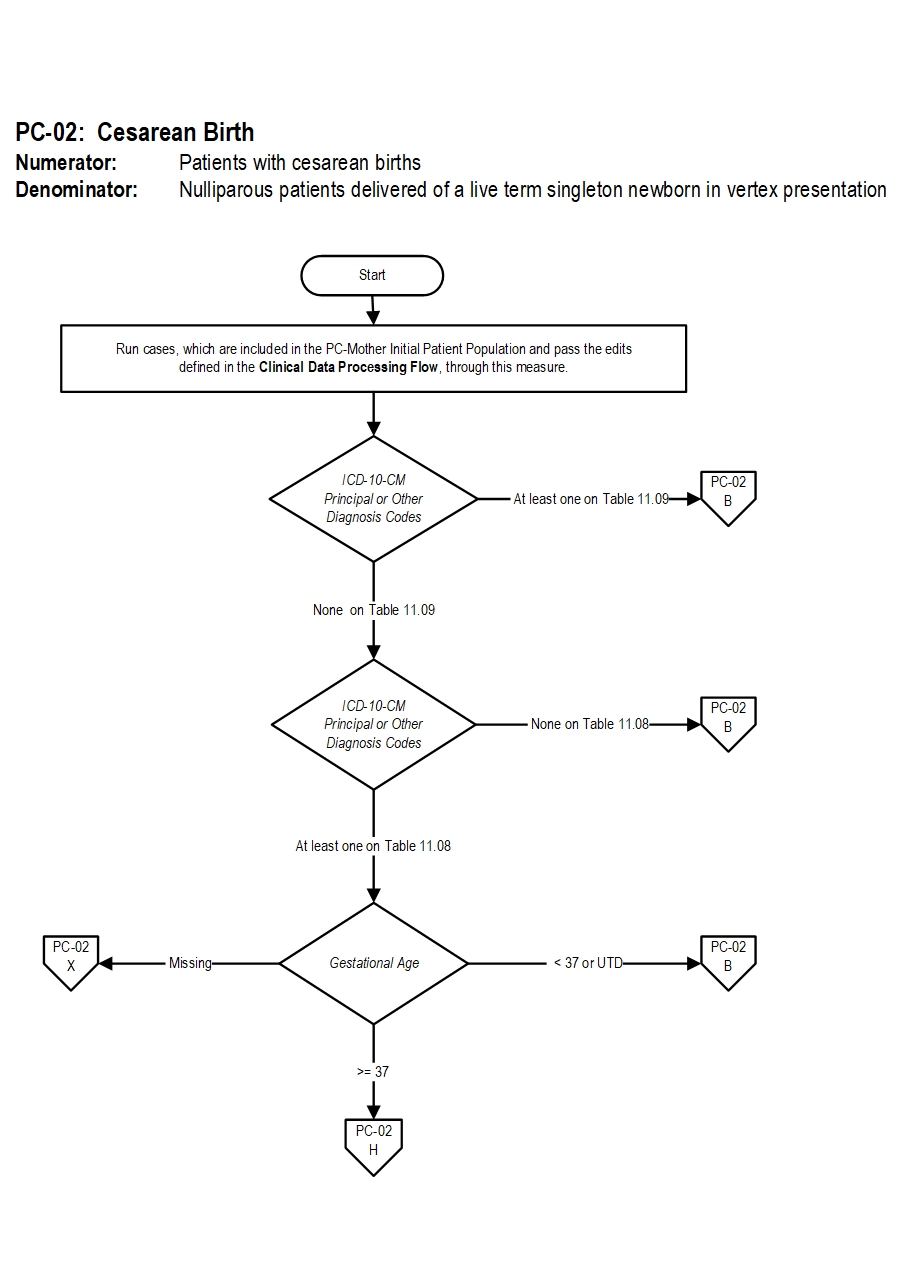
PC-02 Cesarean Birth Algorithm Narrative
Numerator: Patients with cesarean births
Denominator: Nulliparous patients delivered of a live term singleton newborn in vertex presentation
1. Start Cesarean birth logic. Run cases, which are included in the Perinatal Care Mother Initial Patient Population and pass the edits defined in the Clinical Data Processing Flow, through this measure.
2. Check ICD-10 CM Principal or Other Diagnosis codes
- If at least one of the ICD-10 CM Principal or Other Diagnosis codes is on Table 11.09, the case will proceed to a Measure Category Assignment of B and will not be in the Measure Population. Stop processing.
- If all ICD-10 CM Principal or Other Diagnosis codes are missing or none of them on Table 11.09, continue processing and proceed to ICD-10 CM principal or Other Diagnosis Codes.
- If all ICD-10 CM Principal or Other Diagnosis codes are missing or none of them on Table 11.08, the case will proceed to a Measure Category Assignment of B and will not be in the Measure Population. Stop processing.
- If at least one of the ICD-10 CM Principal or Other Diagnosis codes is on Table 11.08, continue processing and proceed to check Gestational Age.
- If the gestational age is missing the case will proceed to a Measure Category Assignment of X and will be rejected. Stop processing.
- If the gestational age is less than 37 weeks or unable to be determined the case will proceed to a Measure Category Assignment of B and will not be in the Measure Population. Stop processing.
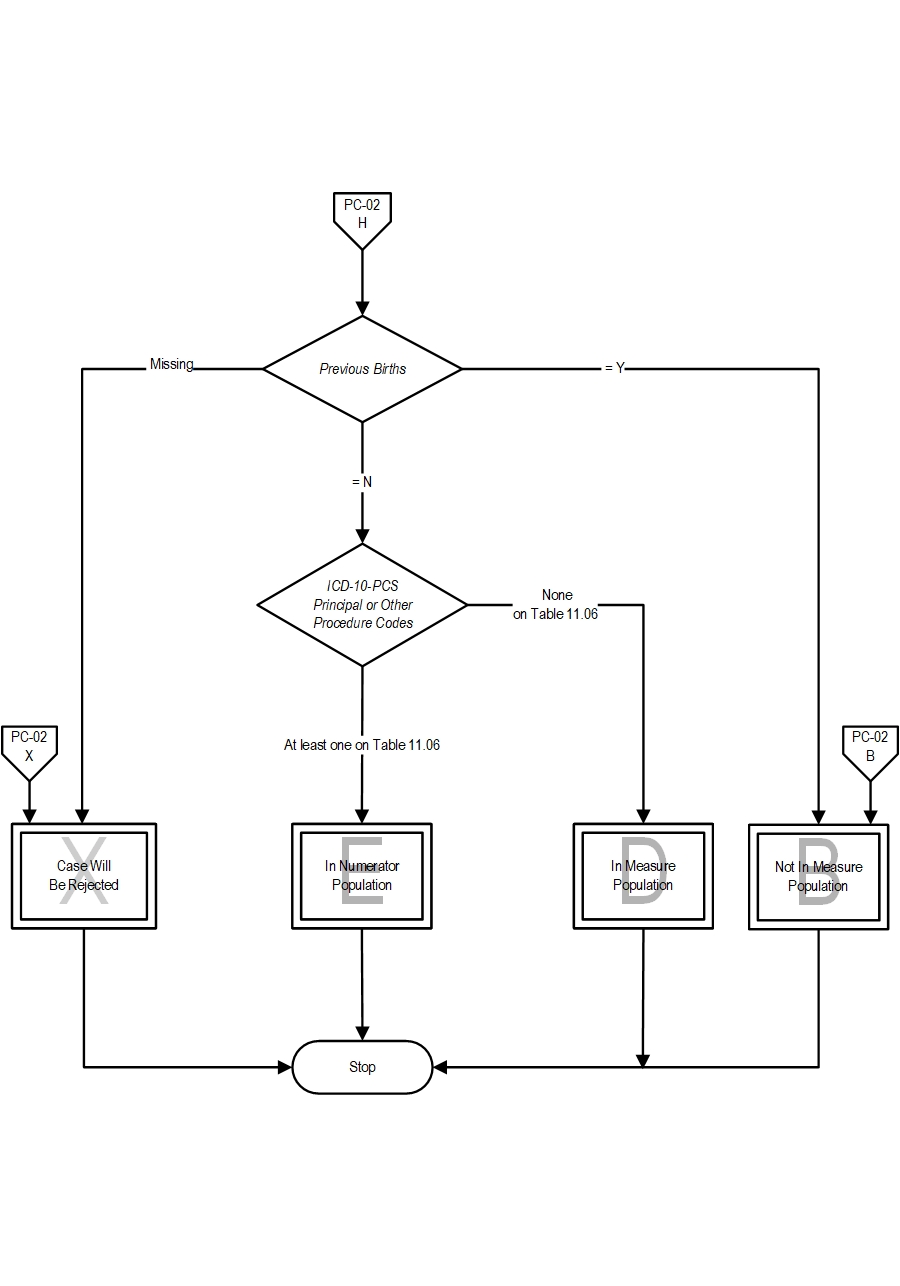
- If the gestational age is greater than or equal to 37 weeks, continue processing and proceed to check Previous Births.
- If previous births is missing, the case will proceed to a Measure Category Assignment of X and will be rejected. Stop processing.
- If previous births is Yes, the case will proceed to a Measure Category Assignment of B and will not be in the Measure Population. Stop processing.
- If previous births is No continue processing and proceed to check ICD-10-PCS principal or other procedure codes.
- If all ICD-10-PCS Principal or Other Procedure Codes are missing or none of them on Table 11.06, the case will proceed to a Measure Category Assignment of D and will be in the population. Stop processing.
- If at least one of the ICD-10-PCS Principal or Other Procedure Codes is on Table 11.06, the case will proceed to a Measure Category Assignment of E and will be in the numerator population. Stop processing.
CPT® only copyright 2023 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association.
You, your employees and agents are authorized to use CPT® only as contained in The Joint Commission performance measures solely for your own personal use in directly participating in healthcare programs administered by The Joint Commission. You acknowledge that the American Medical Association (“AMA”) holds all copyright, trademark and other rights in CPT®.
Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CPT® for resale and/or license, transferring copies of CPT® to any party not bound by this Agreement, creating any modified or derivative work of CPT®, or making any commercial use of CPT®. License to use CPT® for any use not authorized herein must be obtained through the American Medical Association, Intellectual Property Services, AMA Plaza, 330 North Wabash Avenue, Suite 39300, Chicago, Illinois 60611-5885. Applications are available at the American Medical Association Web site, www.ama- assn.org/go/cpt.
U.S. Government Rights This product includes CPT® which is commercial technical data, which was developed exclusively at private expense by the American Medical Association, 330 North Wabash Avenue, Chicago, Illinois 60611. The American Medical Association does not agree to license CPT® to the Federal Government based on the license in FAR 52.227-14 (Data Rights - General) and DFARS 252.227-7015 (Technical Data - Commercial Items) or any other license provision. The American Medical Association reserves all rights to approve any license with any Federal agency.
Disclaimer of Warranties and Liabilities. CPT® is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to the implied warranties of merchantability and fitness for a particular purpose. Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT®, and the (AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this product is with The Joint Commission, and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this product.
This Agreement will terminate upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
Should the foregoing terms and conditions be acceptable to you, please indicate your agreement and acceptance by clicking below on the button labeled “accept”.