Measure Information Form
Version 2023A1
Measure Information Form
The benefits of both IV altelplase and mechanical thrombectomy for the treatment of acute ischemic stroke are time dependent. The earlier the treatment within the time window, the greater the benefit to patients. Initiation of IV alteplase at a primary stroke center (PSC) and rapid transport to an advanced center capable of performing endovascular treatment may lead to faster and more complete reperfusion for certain patients eligible for these treatments (Powers, 2018).
In 2013, The Brain Attack Coalition recommended that stroke transfers occur within 2 hours of patient arrival at the referring stroke center (Alberts, 2013). Since that time, faster door-in-door-out (DIDO) times have been reported for specific groups of stroke patients. For hospitals without an on-site mechanical thrombectomy (MT) service, shorter door-in-door-out (DIDO) times should be the goal. Choi and colleagues recently reported a median DIDO time of 86 minutes (IQR, 65–111) for acute ischemic stroke patients transferred out for potential MT. During working hours (0800–1700 hours), a median DIDO time of 59 minutes (IQR, 51–80) was achieved (Choi, 2019). Prolonged transfer times may result in worse outcomes for MT-eligible patients with evolving large vessel occlusion (ELVO) who are without successful reperfusion. Higher NIHSS scores have been noted at discharge and 90 days (McTaggert, 2018).
Reducing the time stroke patients remain in the emergency department (ED) can improve access to a higher-level of stroke care, surgical intervention, or advanced intra-arterial endovascular treatments, and increase quality of care. For those stroke patients who are not transferred to a TSC or CSC, inpatient admission within 3 hours, preferably to a formal stroke unit, is recommended (Jauch, 2013).
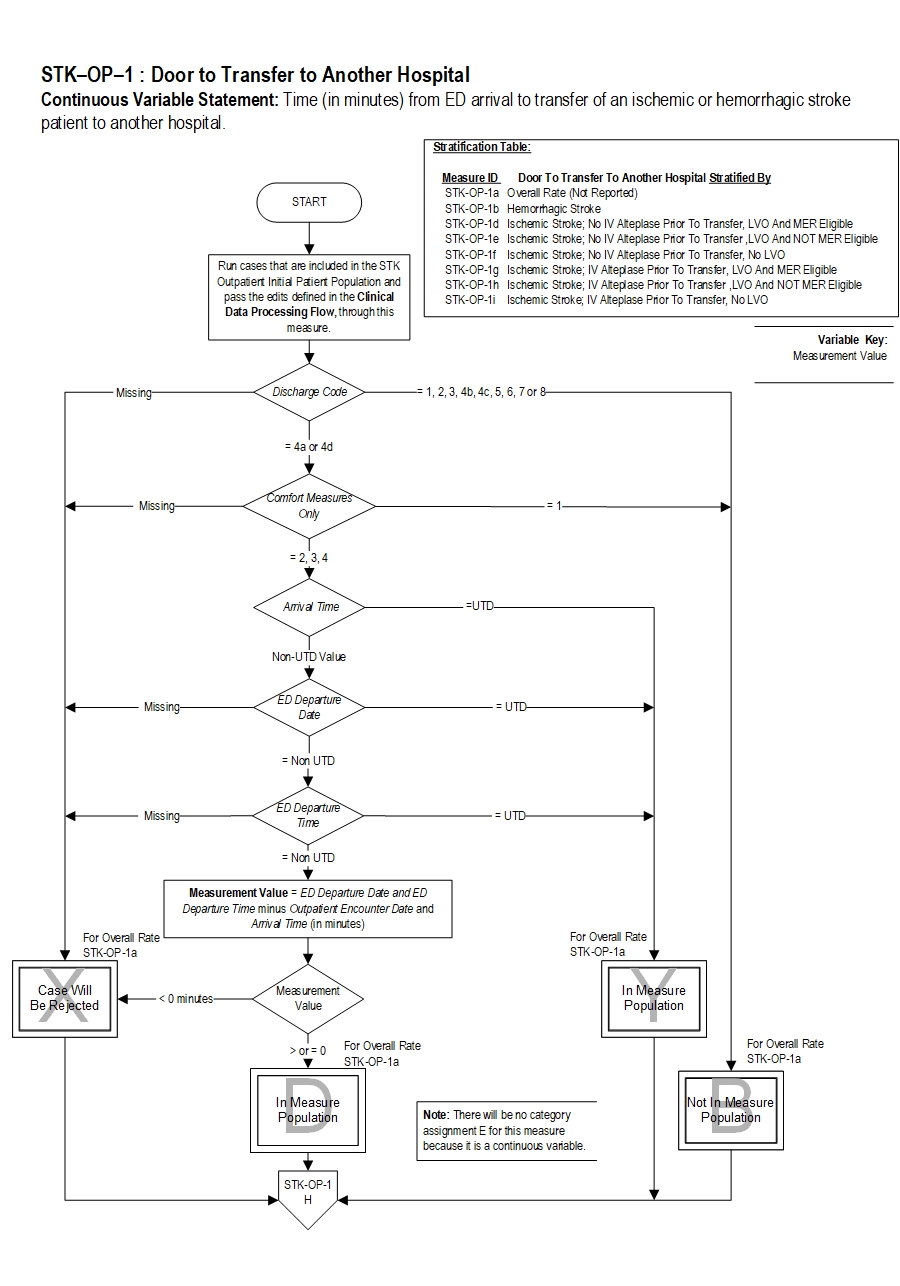
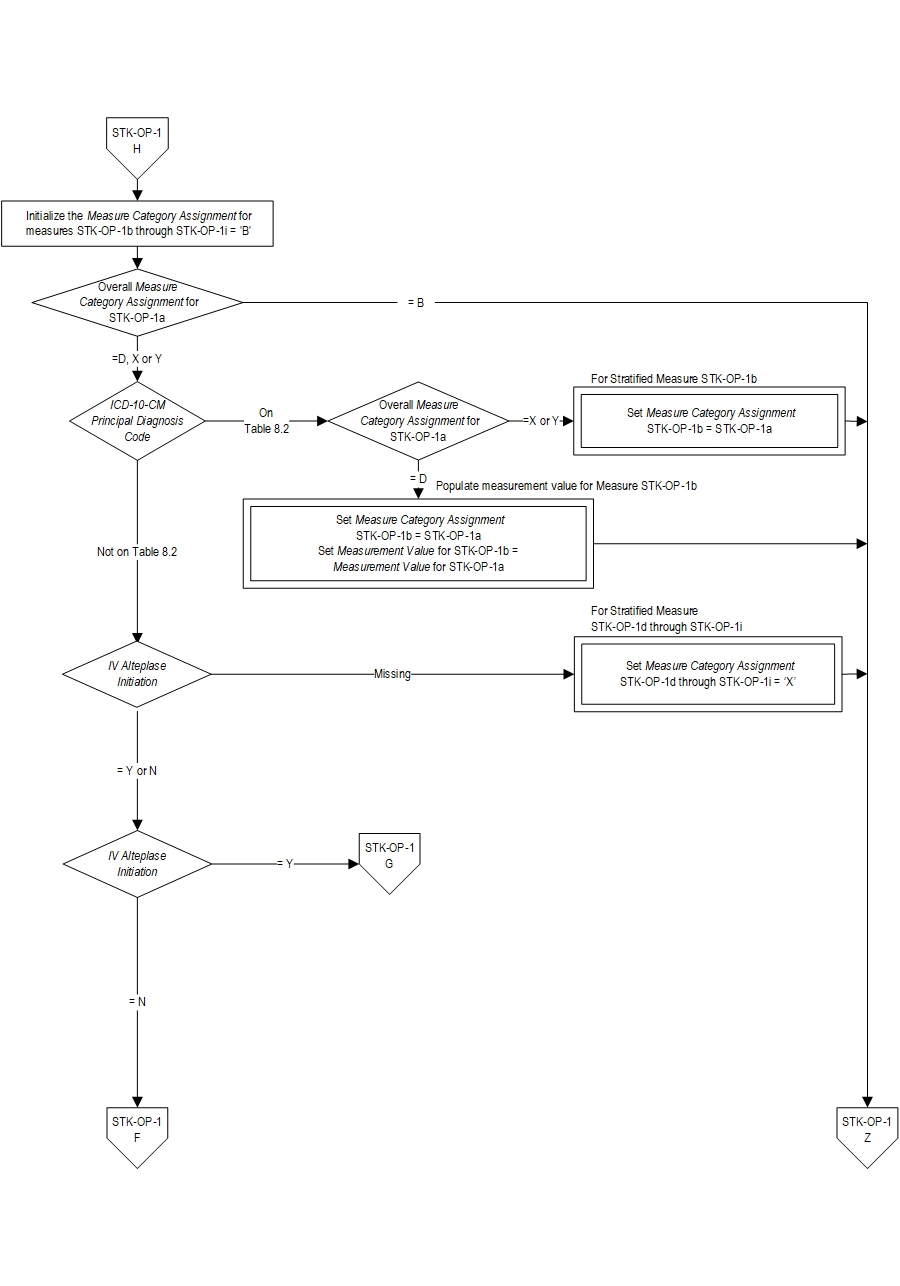
Type Of Measure: Process Improvement Noted As: Decrease in the median valueSTK-OP-1b Time (in minutes) from ED arrival to transfer of a hemorrhagic stroke patient to another hospital
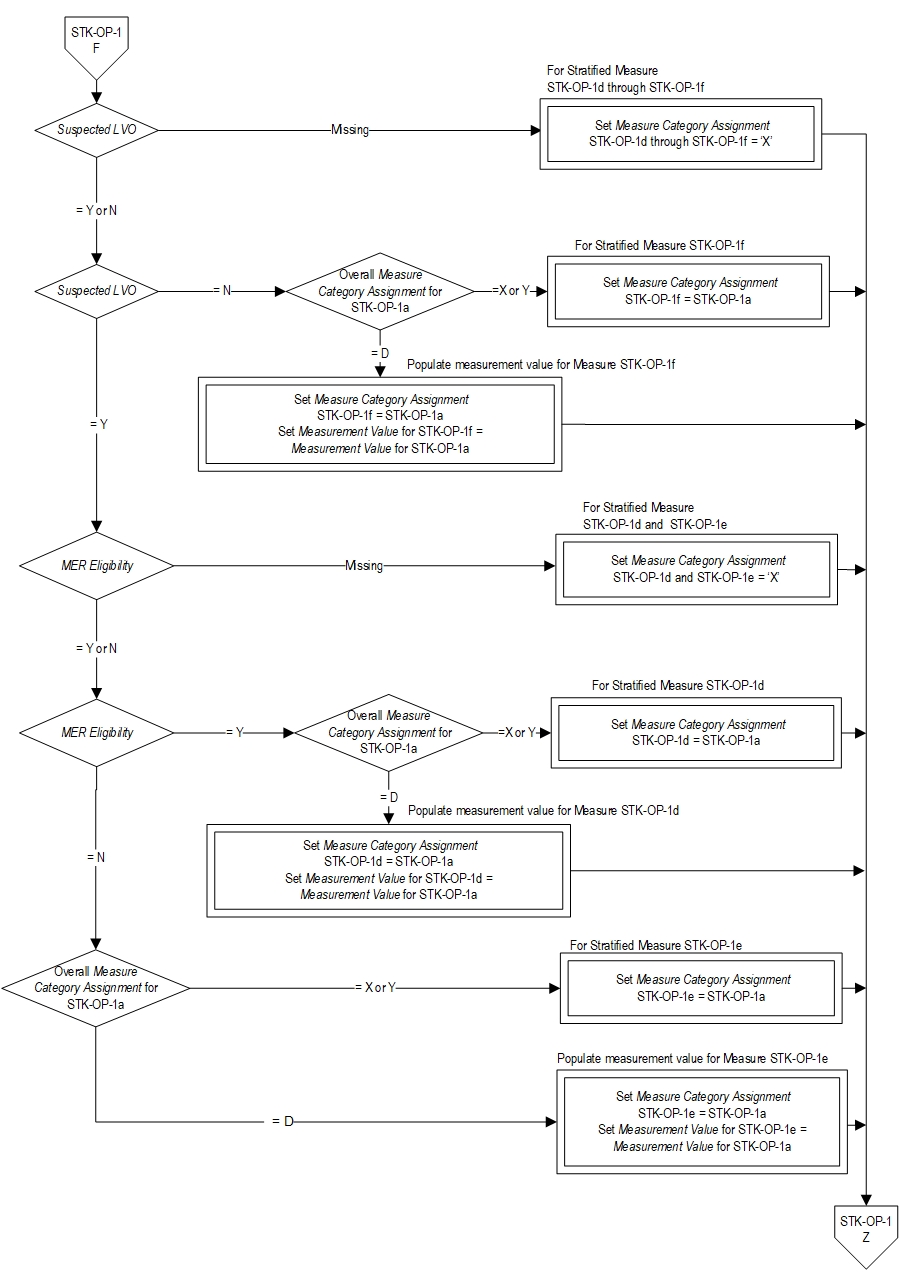
STK-OP-1d Time (in minutes) from ED arrival to transfer of an ischemic stroke patient (no IV alteplase given prior to transfer, LVO and MER eligible) to another hospital
STK-OP-1e Time (in minutes) from ED arrival to transfer of an ischemic stroke patient (no IV alteplase given prior to transfer, LVO and NOT MER eligible) to another hospital
STK-OP-1f Time (in minutes) from ED arrival to transfer of an ischemic stroke patient (no IV alteplase given prior to transfer, no LVO) to another hospital
STK-OP-1g Time (in minutes) from ED arrival to transfer of an ischemic stroke patient (IV alteplase prior to transfer (drip and ship), LVO and MER eligible) to another hospital
STK-OP-1h Time (in minutes) from ED arrival to transfer of an ischemic stroke patient (IV alteplase prior to transfer (drip and ship), LVO and NOT MER eligible) to another hospital
STK-OP-1i Time (in minutes) from ED arrival to transfer of an ischemic stroke patient (IV alteplase prior to transfer (drip and ship), no LVO) to another hospital
Included Populations:AND
- Patients with an ICD-10-CM Principal Diagnosis Code for ischemic or hemorrhagic stroke as defined in Appendix A, Table 8.1 or Table 8.2
AND
- Patients who are transferred to another hospital
Excluded Populations:
- An E/M Code for emergency department encounter as defined in Appendix A, Table 1.0
Data Elements:
- Patients less than 18 years of age
- Patients with Comfort Measures Only documented on day of or day after arrival
- Patients who expired in the emergency department
- Discharges to dispositions other than an acute care facility
- Alberts MJ, Wechsler LR, Jensen MEL, Lachtaw RE, Crocco TJ, George MG, Baranski J, Bass RR, et al. “Formation and Function of Acute Stroke-Ready Hospitals Within a Stroke System of Care Recommendations From the Brain Attack Coalition” [In Eng]. Stroke (Nov 12 2013).
- Albright KC, Branas CC, Meyer BC, Matherne-Meyer DE, Zivin JA, Lyden PD, Carr BG. “Acute Cerebrovascular Care in Emergency Stroke Systems.” [In Eng]. Arch Neurol (Oct 2010).
- American Heart Association. Acute Stroke Ready Hospital, 2015.
- Choi PMC, Tsoi AH, Pope AL, Leung S, Frost T, Loh PS, Chandra RV, Ma T, Parsons M, Mitchell P, Dewey HM. “Door-in-Door-Out Time of 60 Minutes for Stroke With Emergent Large Vessel Occlusion at a Primary Stroke Center.” [In Eng]. Stroke (Aug 29 2019).
- Jauch, E. C., J. L. Saver, H. P. Adams, Jr., A. Bruno, J. J. Connors, B. M. Demaerschalk, P. Khatri, et al. "Guidelines for the Early Management of Patients with Acute Ischemic Stroke: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association." [In Eng]. Stroke (Jan 31 2013).
- Lyerly MJ, Albright KC, Boehme AK, Shahripour RB, Donnelly JP, Houston JT, Rawal PV, Kapoor N, Alvi M, Sisson A, Alexandrov AW, Alexandrov AV. “Patient Selection for Drip and Ship Thrombolysis in Acute Ischemic Stroke”. [In Eng]. South Med J (Jul 2015).
- McTaggert RA, Moldovan K, Oliver LA, Dibiasio EL, Baird GL, Hemendinger ML, Haas RA, Goyal M, Wang TY, Jayaraman MV. “Door-in-Door-Out Time at Primary Stroke Centers May Predict Outcome for Emergent Large Vessel Occlusion Patients.” [In Eng]. Stroke (Nov 8 2018).
- Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, et al; on behalf of the American Heart Association Stroke Council. 2018 Guidelines for the Early Management of Patients with Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2018 Jan;49:e8, e10.
- Sheth KN, Smith EE, Grau-Sepulveda MV, Kleindorfer D, Fonarow GC, Schwamm LH. "Drip and Ship Thrombolytic Therapy for Acute Ischemic Stroke: Use, Temporal Trends, and Outcomes.” [In Eng]. Stoke (Mar 2015).

CPT® only copyright 2022 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association.
You, your employees and agents are authorized to use CPT® only as contained in The Joint Commission performance measures solely for your own personal use in directly participating in healthcare programs administered by The Joint Commission. You acknowledge that the American Medical Association (“AMA”) holds all copyright, trademark and other rights in CPT®.
Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CPT® for resale and/or license, transferring copies of CPT® to any party not bound by this Agreement, creating any modified or derivative work of CPT®, or making any commercial use of CPT®. License to use CPT® for any use not authorized herein must be obtained through the American Medical Association, Intellectual Property Services, AMA Plaza, 330 North Wabash Avenue, Suite 39300, Chicago, Illinois 60611-5885. Applications are available at the American Medical Association Web site, www.ama- assn.org/go/cpt.
U.S. Government Rights This product includes CPT® which is commercial technical data, which was developed exclusively at private expense by the American Medical Association, 330 North Wabash Avenue, Chicago, Illinois 60611. The American Medical Association does not agree to license CPT® to the Federal Government based on the license in FAR 52.227-14 (Data Rights - General) and DFARS 252.227-7015 (Technical Data - Commercial Items) or any other license provision. The American Medical Association reserves all rights to approve any license with any Federal agency.
Disclaimer of Warranties and Liabilities. CPT® is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to the implied warranties of merchantability and fitness for a particular purpose. Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT®, and the (AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this product is with The Joint Commission, and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this product.
This Agreement will terminate upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
Should the foregoing terms and conditions be acceptable to you, please indicate your agreement and acceptance by clicking below on the button labeled “accept”.