Measure Information Form
Version 2020A1
Measure Information Form
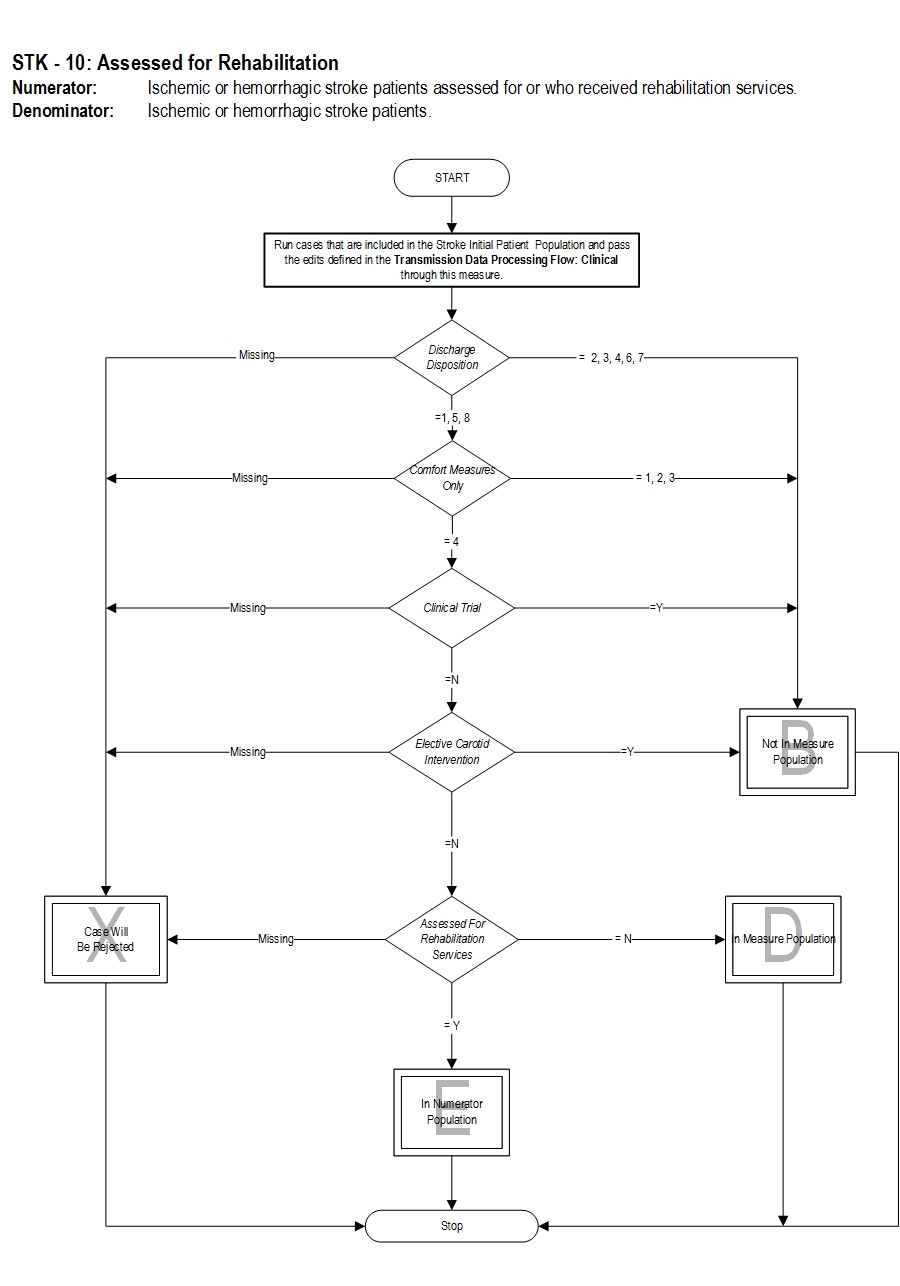
Included Populations: Not applicable Excluded Populations: None Data Elements:Denominator Statement: Ischemic or hemorrhagic stroke patients.
Included Populations: Discharges with an ICD-10-CM Principal Diagnosis Code for ischemic or hemorrhagic stroke as defined in Appendix A, Table 8.1 or Table 8.2. Excluded Populations:Data Elements:
- Patients less than 18 years of age
- Patients who have a Length of Stay greater than 120 days
- Patients with Comfort Measures Only documented
- Patients enrolled in clinical trials
- Patients admitted for Elective Carotid Intervention
- Patients discharged to another hospital
- Patients who left against medical advice
- Patients who expired
- Patients discharged to home for hospice care
- Patients discharged to a health care facility for hospice care
- Bates, B., J. Y. Choi, P. W. Duncan, J. J. Glasberg, G. D. Graham, R. C. Katz, K. Lamberty, et al. "Veterans Affairs/Department of Defense Clinical Practice Guideline for the Management of Adult Stroke Rehabilitation Care: Executive Summary." [In eng]. Stroke 36, no. 9 (Sep 2005): 2049-56.
- Centers for Disease Control and Prevention. "Prevalence and Most Common Causes of Disability among Adults--United States, 2005." [In eng]. MMWR Morb Mortal Wkly Rep 58, no. 16 (May 1 2009): 421-6.
- Duncan, P. W., R. Zorowitz, B. Bates, J. Y. Choi, J. J. Glasberg, G. D. Graham, R. C. Katz, K. Lamberty, and D. Reker. "Management of Adult Stroke Rehabilitation Care: A Clinical Practice Guideline." [In eng]. Stroke 36, no. 9 (Sep 2005): e100-43.
- Foley, N., R. Teasell, S. Bhogal, and M. Speechley. "The Efficacy of Stroke Rehabilitation." In, (2011): 1-50.
- http://www.ebrsr.com/evidence-review/5-efficacy-stroke-rehabilitation
- Gresham, G. E., P. W. Duncan, W. B. Stason, H. P. Adams, A. M. Adelman, D. N. Alexander, D. S. Bishop et al. "Post-stroke rehabilitation. Clinical practice guideline, no. 16. Rockville, MD: US Department of Health and Human Services." Public Health Service, Agency for Health Care Policy and Research (1995): 95-0062.
- Kalra, L., A. Evans, I. Perez, M. Knapp, C. Swift, and N. Donaldson. "A Randomised Controlled Comparison of Alternative Strategies in Stroke Care." [In eng]. Health Technol Assess 9, no. 18 (May 2005): iii-iv, 1-79.
- Keith, R. A. "Rehabilitation after Stroke: Cost-Effectiveness Analyses." [In eng]. J R Soc Med 89, no. 11 (Nov 1996): 631-3.
- Langhorne, P., B. O. Williams, W. Gilchrist, and K. Howie. "Do Stroke Units Save Lives?" [In eng]. Lancet 342, no. 8868 (Aug 14 1993): 395-8.
- "Management of Patients with Stroke: Rehabilitation, Prevention and Management of Complications, and Discharge Planning. A National Clinical Guideline." In, (2002). http://www.nhsggc.org.uk/content/mediaassets/pdf/HSD/sign64.pdf.
- Management of Stroke Rehabilitation Working Group. VA/DoD clinical practice guideline for the management of stroke rehabilitation. Washington (DC): Veterans Health Administration, Department of Defense; 2010.
- Moodie, M., D. Cadilhac, D. Pearce, C. Mihalopoulos, R. Carter, S. Davis, G. Donnan, and Scopes Study Group. "Economic Evaluation of Australian Stroke Services: A Prospective, Multicenter Study Comparing Dedicated Stroke Units with Other Care Modalities." [In eng]. Stroke 37, no. 11 (Nov 2006): 2790-5.
- Noorani, H. Z., B. Brady, L. McGahan, R. Teasell, B. Skidmore, and T. J. Doherty. "Stroke Rehabilitation Services: Systematic Reviews of the Clinical and Economic Evidence." In Ottawa: Canadian Coordinating, Office for Health Technology Assessment, 2003.
- Ottenbacher, K. J., and S. Jannell. "The Results of Clinical Trials in Stroke Rehabilitation Research." [In eng]. Arch Neurol 50, no. 1 (Jan 1993): 37-44.
- "Outcomes in Stroke Rehabilitation." Topics in Stroke Rehabilitation 12, no. 4 (Fall 2005): 1-10, 11-19, 20-27, 28-36, 37-49.
- Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, et al; on behalf of the American Heart Association Stroke Council. 2018 Guidelines for the Early Management of Patients with Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2018 Jan;49:e39.
- "Rehabilitation Helps Stroke Patients Recover Skills ". American Academy of Physical Medicine and Rehabilitation, http://www.aapmr.org/patients/conditions/neurologic/Pages/recover.aspx.
- Saka, O., V. Serra, Y. Samyshkin, A. McGuire, and C. C. Wolfe. "Cost-Effectiveness of Stroke Unit Care Followed by Early Supported Discharge." [In eng]. Stroke 40, no. 1 (Jan 2009): 24-9.
- Stroke, National Institute of Neurological Disorders and. "Post-Stroke Rehabilitation Fact Sheet." http://www.ninds.nih.gov/disorders/stroke/poststrokerehab.htm.
- "Urgency Key but Perseverance Pays Off." American Academy of Physical Medicine and Rehabilitation. http://www.zoominfo.com/CachedPage/?archive_id=0&page_id=389260562&page_url=//www.aapmr.org/condtreat/rehab/strokeusa.htm&page_last_updated=2010-07-28T02:27:25&firstName=Charles&lastName=Levy
CPT® only copyright 2019 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association.
You, your employees and agents are authorized to use CPT® only as contained in The Joint Commission performance measures solely for your own personal use in directly participating in healthcare programs administered by The Joint Commission. You acknowledge that the American Medical Association (“AMA”) holds all copyright, trademark and other rights in CPT®.
Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CPT® for resale and/or license, transferring copies of CPT® to any party not bound by this Agreement, creating any modified or derivative work of CPT®, or making any commercial use of CPT®. License to use CPT® for any use not authorized herein must be obtained through the American Medical Association, Intellectual Property Services, AMA Plaza, 330 North Wabash Avenue, Suite 39300, Chicago, Illinois 60611-5885. Applications are available at the American Medical Association Web site, www.ama- assn.org/go/cpt.
U.S. Government Rights This product includes CPT® which is commercial technical data, which was developed exclusively at private expense by the American Medical Association, 330 North Wabash Avenue, Chicago, Illinois 60611. The American Medical Association does not agree to license CPT® to the Federal Government based on the license in FAR 52.227-14 (Data Rights - General) and DFARS 252.227-7015 (Technical Data - Commercial Items) or any other license provision. The American Medical Association reserves all rights to approve any license with any Federal agency.
Disclaimer of Warranties and Liabilities. CPT® is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to the implied warranties of merchantability and fitness for a particular purpose. Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT®, and the (AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this product is with The Joint Commission, and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this product.
This Agreement will terminate upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
Should the foregoing terms and conditions be acceptable to you, please indicate your agreement and acceptance by clicking below on the button labeled “accept”.