Measure Information Form
Version 2020A
Measure Information Form
The incidence of health care-associated bacteremia increases with decreasing birth weight. Other risk factors include central venous catheter use, prolonged time using parenteral nutrition, prolonged time on mechanical ventilation, use of H2-blocking agents, and overcrowding or heavy staff loads (Adams-Chapman & Stoll, 2002; Barton et al., 1999; Gaynes et al., 1996; Stoll et al., 2002). The most common causative organisms are coagulase-negative staphylococci, Staphylococcus aureus, enterococci, Enterobacter sp, and Escherichia coli (Adams-Chapman & Stoll, 2002; Clark et al., 2004b; Gaynes et al., 1996; Horbar et al., 2001; Payne et al., 2004; Sohn et al., 2001; Stoll et al., 2002).
Effective preventive measures range from simple hand-washing protocols or closed medication delivery systems to more elaborate multidisciplinary quality improvement plans involving hand-washing, nutrition, skin care, respiratory care, vascular access, and diagnostic practices. All of these interventions have been shown to substantially reduce infection rates, albeit in nonrandomized studies using historical or concurrent control units (Adams-Chapman & Stoll, 2002; Aly et al., 2005; Bloom et al., 2003; Clark et al., 2004a; Clark et al., 2004b; Horbar et al., 2001; Lam et al., 2004; Kilbride et al., 2003a; Kilbride et al., 2003b; Ng et al., 2004; Schelonka et al., 2006). For example, six Vermont Oxford Network NICUs reduced their rates of coagulase-negative staphylococcus infections from 22.0% in 1994 to 16.6% in 1996 after implementing a quality improvement model (versus a much smaller decrease from 15.4% to 14.5% at 66 comparison NICUs) (Horbar et al., 2001). A similar reduction from 24.6% to 16.4% was achieved with a multi-modality, multi-hospital intervention focusing on hand hygiene with an effective agent before and after every patient contact, eliminating hand jewelry and artificial nails, using maximal barrier precautions during central venous catheter insertion, decreasing the number of skin punctures, reducing the duration of intravenous lipid and deep line use, and improving the diagnosis of health care-associated infections. (Kilbride et al., 2003a; Kilbride et al., 2003b).
Given the fragility and susceptibility of the patient population, a baseline level of health care-associated infections will be expected, even with good protocols in place. However, those centers that have prevention protocols, and are able to encourage health care workers to adhere to these protocols, will probably have success in reducing their rates of health care-associated bacteremia in their neonatal population. Indeed, several quasi-experimental studies have demonstrated that NICUs can lower their infection rates (based on positive blood cultures) from as high as 13.5 per 1,000 patient days to as low as 3.0 per 1,000 patient days( Adams-Chapman & Stoll, 2002; Aly et al., 2005; Bloom et al. ,2003; Clark et al., 2004a; Clark et al., 2004b; Horbar et al., 2001; Lam et al., 2004; Kilbride et al., 2003a; Kilbride et al., 2003b; Ng et al., 2004; Schelonka et al., 2006).
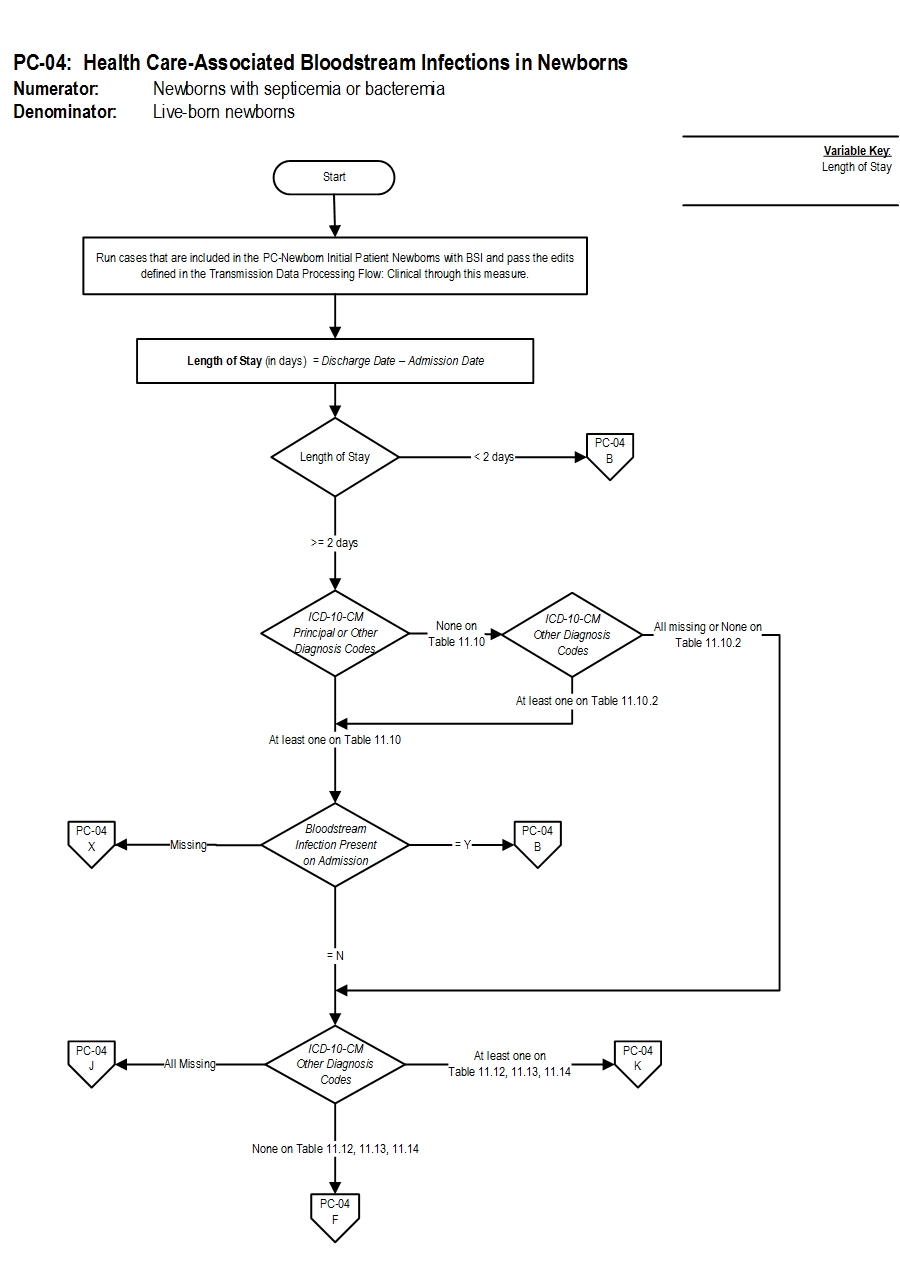
Type Of Measure: Outcome Improvement Noted As: Decrease in the rateIncluded Populations:Denominator Statement: Liveborn newborns
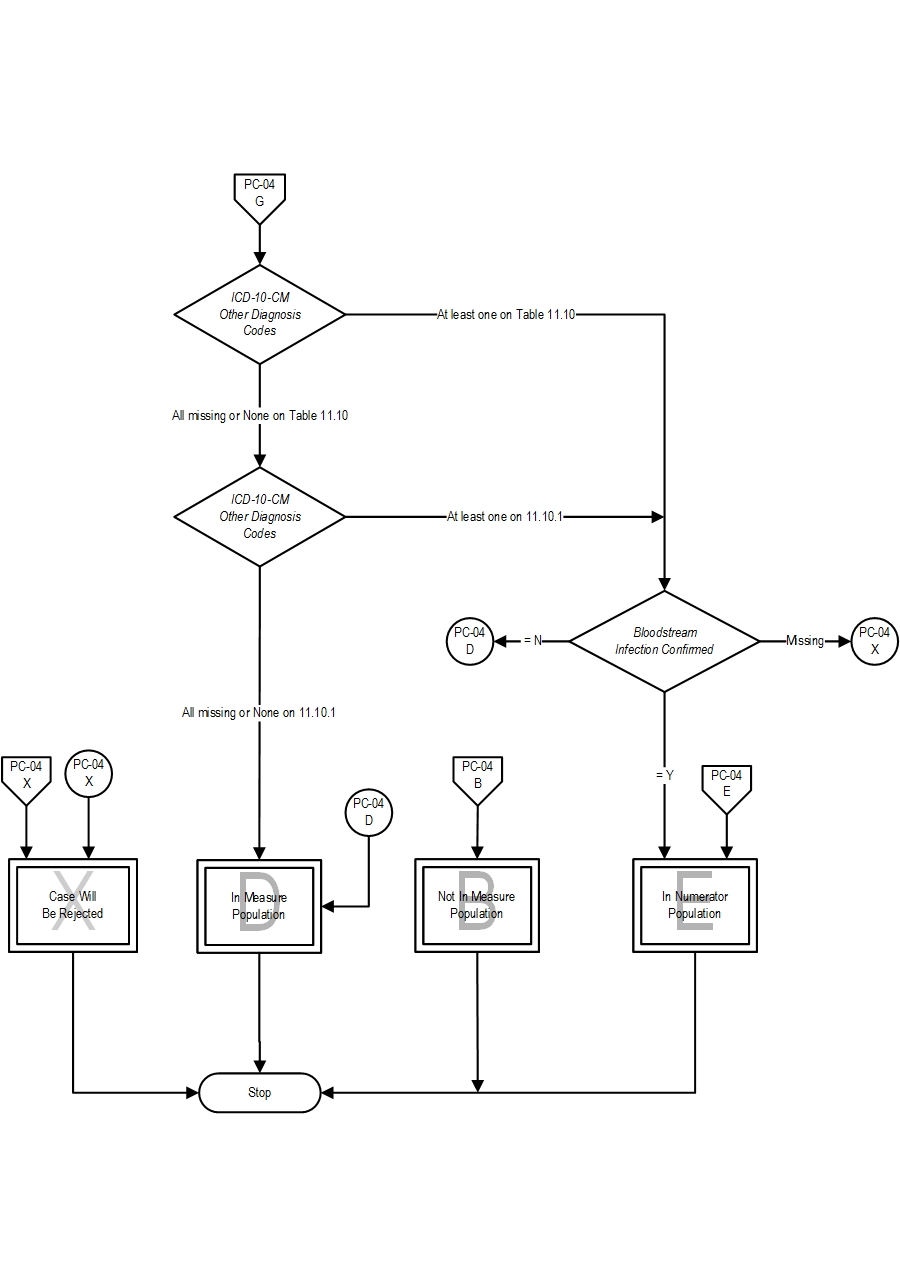
- ICD-10-CM Other Diagnosis Codes for newborn septicemia or bacteremia as defined in Appendix A, Table 11.10 with a Bloodstream Infection Confirmed
OR
Excluded Populations: None Data Elements:
- ICD-10-CM Other Diagnosis Codes for sepsis as defined in Appendix A, Table 11.10.1 with a Bloodstream Infection Confirmed
Included Populations:OR
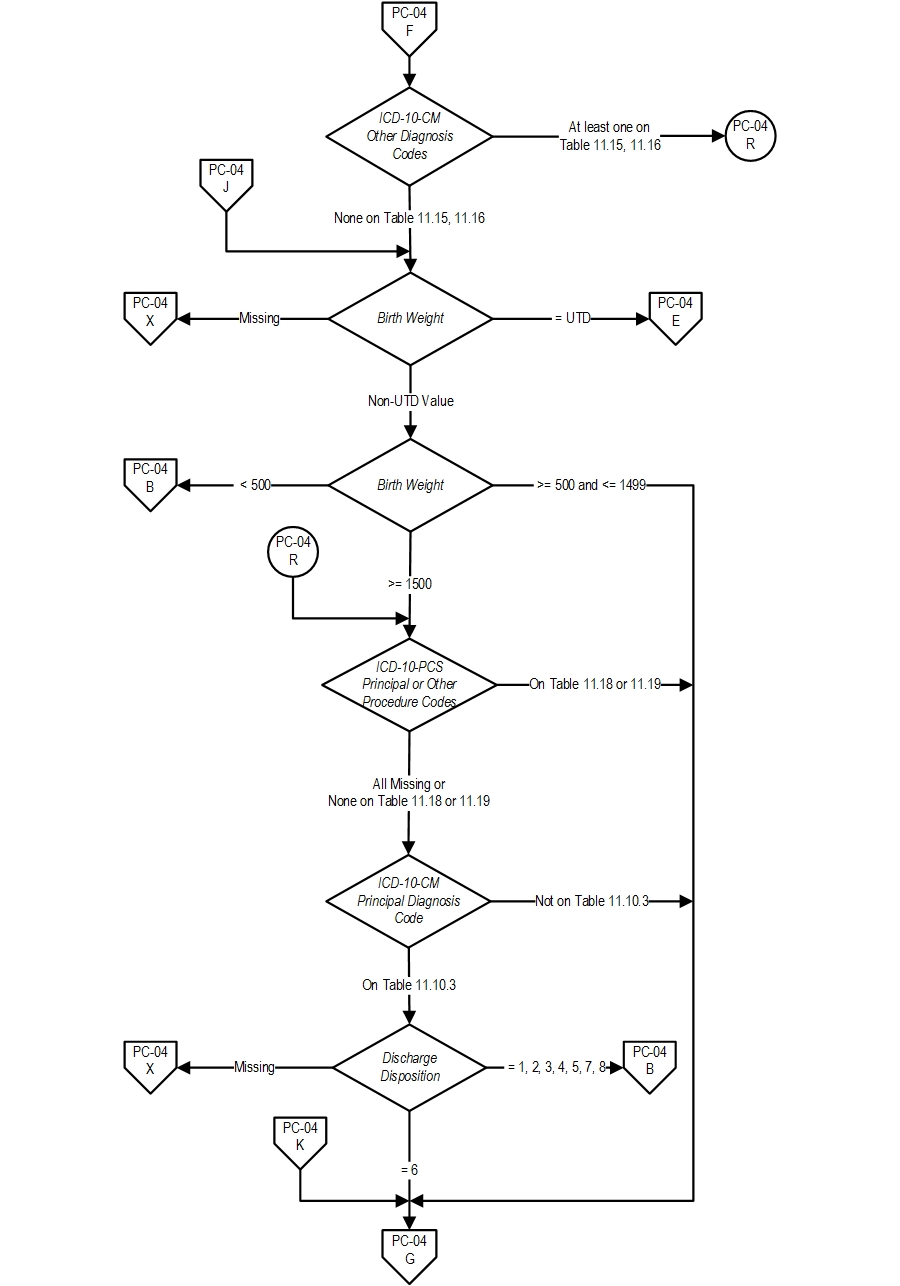
- ICD-10-CM Other Diagnosis Codes for birth weight between 500 and 1499g as defined in Appendix A, Table 11.12, 11.13 or 11.14 OR Birth Weight between 500 and 1499g
Excluded Populations:
- ICD-10-CM Other Diagnosis Codes for birth weight ≥ 1500g as defined in Appendix A, Table 11.15 or 11.16 OR Birth Weight ≥ 1500g who experienced one or more of the following:
- Experienced death
- ICD-10-PCS Principal Procedure Code or ICD-10-PCS Other Procedure Codes for major surgery as defined in Appendix A, Table 11.18
- ICD-10-PCS Principal Procedure Code or ICD-10-PCS Other Procedure Codes for mechanical ventilation as defined in Appendix A, Table 11.19
- Transferred in from another acute care hospital or health care setting within 2 days of birth
Data Elements:
- ICD-10-CM Principal Diagnosis Code for septicemias or bacteremias as defined in Appendix A, Table 11.10.2
- ICD-10-CM Other Diagnosis Codes for septicemias or bacteremias as defined in Appendix A, Table 11.10.2 or ICD-10-CM Principal or Other Diagnosis Codes for newborn septicemia or bacteremia as defined in Appendix A, Table 11.10 with a Bloodstream Infection Present on Admission
- ICD-10-CM Other Diagnosis Codes for birth weight < 500g as defined in Appendix A, Table 11.20 OR Birth Weight < 500g
- Length of Stay < 2 days
Data Elements:Data Collection Approach: Retrospective data sources for required data elements include administrative data and medical records. Data Accuracy:
- Variation may exist in the assignment of ICD-10 codes; therefore, coding practices may require evaluation to ensure consistency.
- Since Birth Weight is a risk factor for hospital associated blood stream infections in newborns, ICD-10-CM codes have been provided in Appendix A, Tables 11.12-11.16, 11.20 to assist in identifying newborns with prematurity and fetal growth retardation to denote birth weight (less than 500 grams up to birth weight 2000-2499 grams). Therefore, newborns with birth weights greater than or equal to 2500 grams will need to be captured using the data element Birth Weight.
- It is important to ensure that all weight conversions from pounds and ounces to grams are accurate and concise. Birth Weight should not be rounded off i.e., when converting from pounds and ounces to grams, do not round to the nearest pound before converting the weight to grams.
- Discrepancies can occur between Birth Weights obtained from labor and delivery vs. nursery departments. Organizations should determine which is the most reliable source for this data element value and consistently obtain it from that source.
- Adams-Chapman, I. & Stoll, B.J. (2002). Prevention of nosocomial infections in the neonatal intensive care unit. Current Opinion in Pediatrics.14 (2):157-64.
- Aly, H., Herson, V., Duncan, A., et al. (2005). Is bloodstream infection preventable among premature infants? A tale of two cities. Pediatrics. 115(6):1513-8.
- Barton, L., Hodgman, J.E., & Pavlova, Z. (1999). Causes of death in the extremely low birth weight infant. Pediatrics. 103(2):446-51.
- Bloom, B.T., Craddock, A., Delmore, P.M., et al. (2003). Reducing acquired infections in the NICU: observing and implementing meaningful differences in process between high and low acquired infection rate centers. Journal of Perinatology. 23(6):489-92.
- Clark, R., Powers, R., White, R., Bloom, B., Sanchez, P., & Benjamin, D.K., Jr. (2004a). Prevention and treatment of nosocomial sepsis in the NICU. Journal of Perinatology. 4; 24(7):446-53.
- Clark, R., Powers, R., White, R., Bloom, B., Sanchez, P., & Benjamin, D.K., Jr. (2004b). Nosocomial infection in the NICU: a medical complication or unavoidable problem? Journal of Perinatology. 24(6):382-8.
- Gaynes, R.P., Edwards, J.R., Jarvis, W.R., Culver, D.H., Tolson, J.S., & Martone, W.J. (1996). Nosocomial infections among neonates in high-risk nurseries in the United States. National Nosocomial Infections Surveillance System. Pediatrics. 98(3 Pt 1):357-61.
- Horbar, J.D., Rogowski, J., Plsek, P.E., et al. (2001). Collaborative quality improvement for neonatal intensive care. NIC/Q Project Investigators of the Vermont Oxford Network. Pediatrics. 107(1):14-22.
- Kilbride, H.W., Wirtschafter, D.D., Powers, R.J., & Sheehan, M.B. (2003a). Implementation of evidence-based potentially better practices to decrease nosocomial infections. Pediatrics. 111(4 Pt 2):e519-33.
- Kilbride, H.W., Powers, R., Wirtschafter, D.D., et al. (2003b). Evaluation and development of potentially better practices to prevent neonatal nosocomial bacteremia. Pediatrics. 111(4 Pt 2):e504-18.
- Lam, B.C., Lee, J., & Lau, Y.L. (2004). Hand Hygiene Practices in a Neonatal Intensive Care Unit: A Multimodal Intervention and Impact on Nosocomial Infection. Pediatrics.114 (5):e565.
- Ng, P.C., Wong, H.L., Lyon, D.J., et al. (2004). Combined use of alcohol hand rub and gloves reduces the incidence of late onset infection in very low birthweight infants. Archives of Disease in Childhood Fetal & Neonatal Edition. 89(4):F336-40.
- Payne, N.R., Carpenter, J.H., Badger, G.J., Horbar, J.D., & Rogowski, J. (2004). Marginal increase in cost and excess length of stay associated with nosocomial bloodstream infections in surviving very low birth weight infants. Pediatrics. 114(2):348-55.
- Schelonka, R.L., Scruggs, S., Nichols, K., Dimmitt, R.A., & Carlo, W.A. (2006). Sustained reductions in neonatal nosocomial infection rates following a comprehensive infection control intervention. Journal of Perinatology. 26(3):176-9.
- Sohn, A.H., Garrett, D.O., Sinkowitz-Cochran, R.L., et al. (2001). Prevalence of nosocomial infections in neonatal intensive care unit patients: Results from the first national point-prevalence survey. Journal of Pediatrics. 139(6):821-7.
- Stoll, B.J., Hansen, N., Fanaroff, A.A., et al. (2002). Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics. 110(2 Pt 1):285-91.
Agency for Healthcare Research and Quality
CPT® only copyright 2019 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association.
You, your employees and agents are authorized to use CPT® only as contained in The Joint Commission performance measures solely for your own personal use in directly participating in healthcare programs administered by The Joint Commission. You acknowledge that the American Medical Association (“AMA”) holds all copyright, trademark and other rights in CPT®.
Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CPT® for resale and/or license, transferring copies of CPT® to any party not bound by this Agreement, creating any modified or derivative work of CPT®, or making any commercial use of CPT®. License to use CPT® for any use not authorized herein must be obtained through the American Medical Association, Intellectual Property Services, AMA Plaza, 330 North Wabash Avenue, Suite 39300, Chicago, Illinois 60611-5885. Applications are available at the American Medical Association Web site, www.ama- assn.org/go/cpt.
U.S. Government Rights This product includes CPT® which is commercial technical data, which was developed exclusively at private expense by the American Medical Association, 330 North Wabash Avenue, Chicago, Illinois 60611. The American Medical Association does not agree to license CPT® to the Federal Government based on the license in FAR 52.227-14 (Data Rights - General) and DFARS 252.227-7015 (Technical Data - Commercial Items) or any other license provision. The American Medical Association reserves all rights to approve any license with any Federal agency.
Disclaimer of Warranties and Liabilities. CPT® is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to the implied warranties of merchantability and fitness for a particular purpose. Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT®, and the (AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this product is with The Joint Commission, and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this product.
This Agreement will terminate upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
Should the foregoing terms and conditions be acceptable to you, please indicate your agreement and acceptance by clicking below on the button labeled “accept”.