Release Notes:
Measure Information Form
Version 2018A
Measure Information Form
Version 2018A
Measure Information Form
The National Consensus Project for Quality Palliative Care (2013) guidelines recommend that patient’s or surrogate’s goals, preferences, and choices be respected and used as the basis for the plan of care within the limits of laws and standards of care. The palliative care interdisciplinary team discusses achievable goals with the patient and family using a patient-centered approach that includes the patient values and preferences and assists with advance care planning documents to communicate patient preferences across care settings
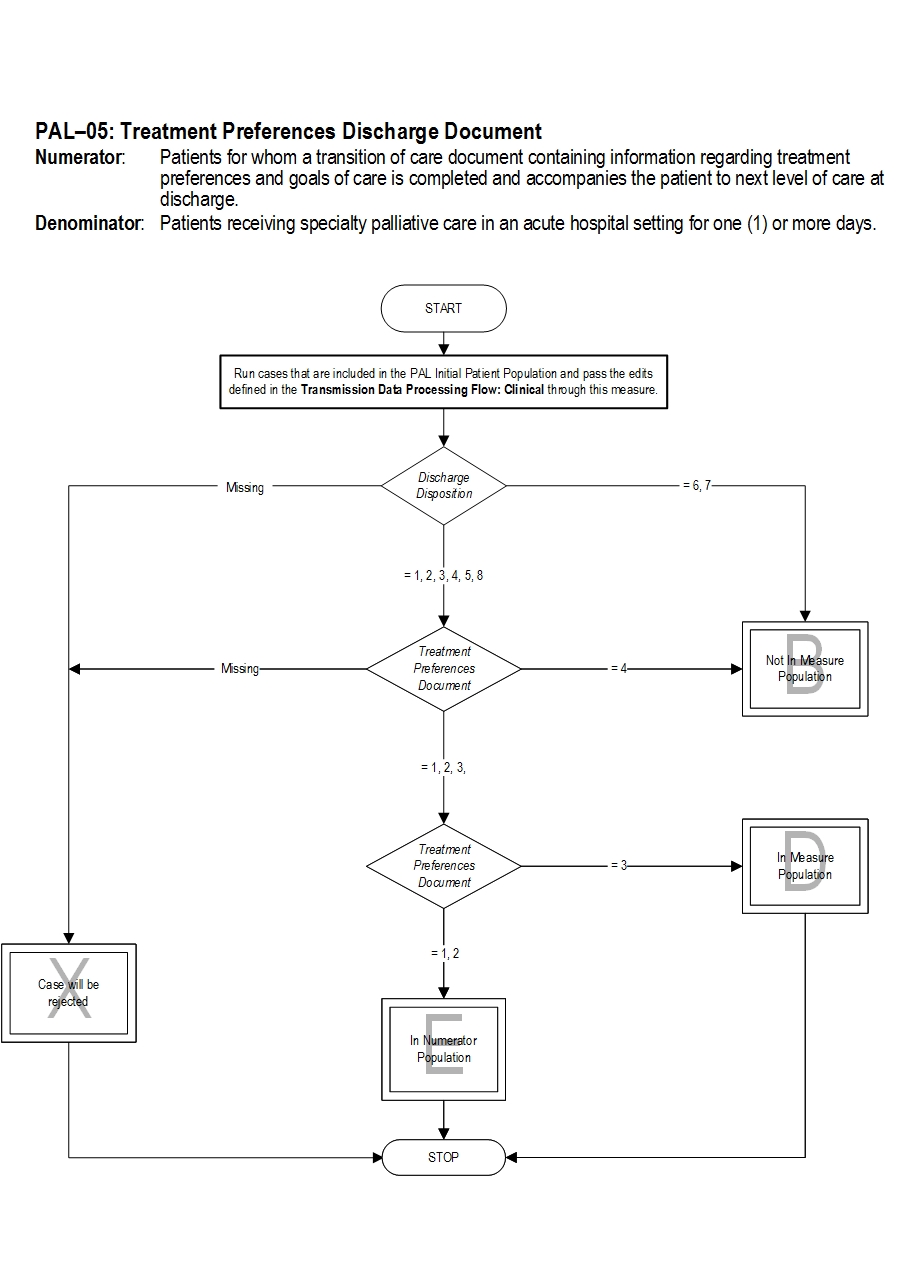
Type of Measure: Process Improvement Noted As: Increase in the rate Numerator Statement: Patients for whom a transition of care document containing information regarding treatment preferences and goals of care is completed and accompanies the patient to the next level of care at discharge.
Risk Adjustment: No.
Data Collection Approach: Retrospective data sources for required data elements include administrative data and medical records. Some hospitals may prefer to gather data concurrently by identifying patients in the population of interest. This approach provides opportunities for improvement at the point of care/service. However, complete documentation includes the principal or other ICD-10CM/PCS diagnosis and procedure codes, which require retrospective data entry.
Data Accuracy: Variation may exist in the assignment of ICD-10CM/PCS codes; therefore, coding practices may require evaluation to ensure consistency.
Measure Analysis Suggestions: None
Sampling: Yes. Please refer to the measure set specific sampling requirements and for additional information see the Population and Sampling Specifications Section.
Data Reported As: Aggregate rate generated from count data reported as a proportion.
Selected References: Included Populations: Not applicable Excluded Populations: None Data Elements:Denominator Statement: Patients receiving specialty palliative care in an acute hospital setting for one (1) or more days
Included Populations: Excluded Populations:Data Elements:
- Patients with discharge disposition of expired or left against medical advice/AMA
- CMS Hospice Item Set, http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Hospice-Quality-Reporting/Hospice-Item-Set-HIS.html
- Field MJ, Cassell CK eds. Approaching Death: Improving Care at the End of Life. Washington, DC: National Academy Press, 1997.
- Gysels M, Richardson A, Higginson I. Communication training for health professionals who care for patients with cancer: a systematic review of effectiveness. Support Care Cancer 2004; 12:692-700.
- Hancock K, Clayton JM, Parker SM et al. Discrepant perceptions of end-of-life communication: a systematic review. J Pain Symptom Manage 2007; 34: 190-200.
- Measuring What Matters, http://aahpm.org/quality/measuring-what-matters
- PEACE Hospice and Palliative Care Quality Measures, http://www.med.unc.edu/pcare/resources/PEACE-Quality-Measures
- Steinhauser KE, Christakis NA, Clipp EC et al. Preparing for the end of life: references of patients, families, physicians and other care providers. J Pain Symptom Manage 2001; 22:727-737.
- SUPPORT Principal Investigators. A controlled trial to improve care for seriously ill hospitalized patients: the Study to Understand Prognosis and Preferences for Outcomes and Risks of Treatments (SUPPORT). JAMA 1995; 274:1591-1598.
- National Consensus Project for Quality Palliative Care. Clinical Practice Guidelines for Quality Palliative Care. 3rd ed. Pittsburgh, PA: Author; 2013. http://www.nationalconsensusproject.org/NCP_Clinical_Practice_Guidelines_3rd_Edition.pdf
American Academy of Hospice and Palliative Care (AAHPM) and Hospice and Palliative Nurses Association (HPNA) Measuring What Matters Project Top Ten Measures That Matter List
PEACE Hospice and Palliative Care Quality Measures Set Measure Algorithm:
| Related Topics |
Questions? Ask Question to Joint Commission staff
Copyright © 2018 by The Joint Commission.