Release Notes:
Measure Information Form
Version 2018A
Measure Information Form
Version 2018A
Measure Information Form
National Consensus Project for Quality Palliative Care (2013) guidelines recommend that the interdisciplinary team assesses and manages pain in a safe and timely manner to a level acceptable to the patient or surrogate and that symptom assessment, treatment, side effect and treatment outcome information should be recorded in the medical record
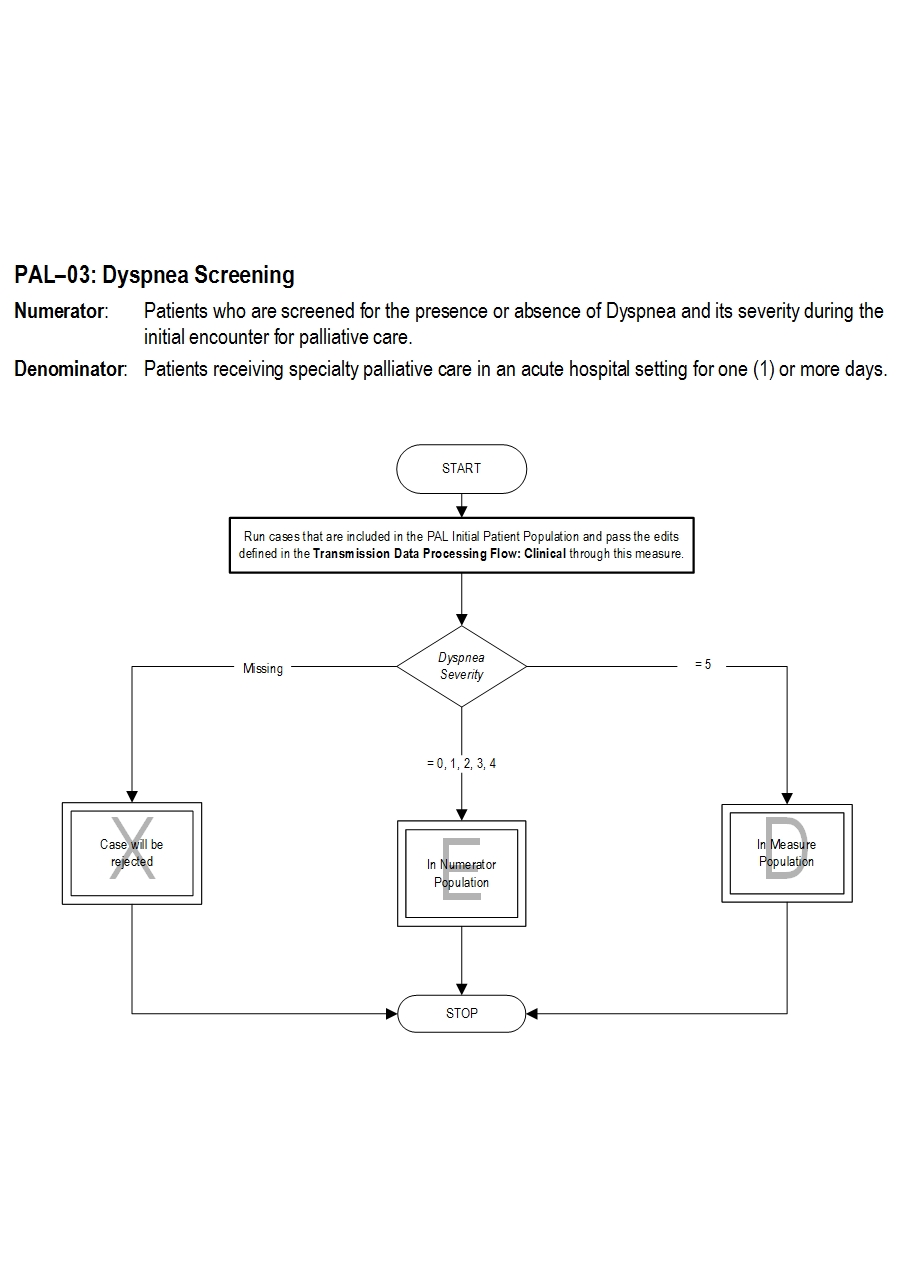
Type of Measure: Process Improvement Noted As: Increase in the rate Numerator Statement: Patients who are screened for the presence or absence of Dyspnea and its severity during the initial encounter for palliative care.
Risk Adjustment: No.
Data Collection Approach: Retrospective data sources for required data elements include administrative data and medical records. Some hospitals may prefer to gather data concurrently by identifying patients in the population of interest. This approach provides opportunities for improvement at the point of care/service. However, complete documentation includes the principal or other ICD-10CM/PCS diagnosis and procedure codes, which require retrospective data entry.
Data Accuracy: Variation may exist in the assignment of ICD-10CM/PCS codes; therefore, coding practices may require evaluation to ensure consistency.
Measure Analysis Suggestions: None
Sampling: Yes. Please refer to the measure set specific sampling requirements and for additional information see the Population and Sampling Specifications Section.
Data Reported As: Aggregate rate generated from count data reported as a proportion.
Selected References: Included Populations: Not applicable Excluded Populations: None Data Elements:Denominator Statement: Patients receiving specialty palliative care in an acute hospital setting for one (1) or more days
Included Populations: Excluded Populations:Data Elements:
- Palliative care program length of stay less than one (1) day
- Bausewin C, Booth S, Gysels M et al. Non-pharmacologic interventions for breathlessness in advanced stages of malignant and nonmalignant diseases. Cochrane Database Syst Rev 2009. Apr 16; 2:CD005623.
- Ben-Aharon I, Gafter-Gvili A, Paul M et al. Interventions for alleviating cancer-related dyspnea: a systematic review. J Clin Oncol 2008; 26:2396-2404.
- CMS Hospice Item Set, http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Hospice-Quality-Reporting/Hospice-Item-Set-HIS.html
- Currow DC, Ward AM, Abernethy AP. Advances in the pharmacologic management of breathlessness. Current Opin Supp Pall Care 2009; 3:103-106.
- Dy SM, Lorenz KA, Naeim A et al. Evidence-based recommendations for cancer fatigue, anorexia, depression and dyspnea. J Clin Onc 2008; 26:3886-3895.
- Lorenz KA, Lynn J, Dy SM et al. Evidence for improving palliative care at the end of life: a systematic review. Ann Intern Med 2008; 148:147-159.
- Luce JM, Luce JA. Management of dyspnea in patients with far-advanced lung disease. JAMA 2001; 285:1331-1337.
- Measuring What Matters, http://aahpm.org/quality/measuring-what-matters
- National Consensus Project for Quality Palliative Care. Clinical Practice Guidelines for Quality Palliative Care. 3rd ed. Pittsburgh, PA: Author; 2013. http://www.nationalconsensusproject.org/NCP_Clinical_Practice_Guidelines_3rd_Edition.pdf
- PEACE Hospice and Palliative Care Quality Measures, http://www.med.unc.edu/pcare/resources/PEACE-Quality-Measures
- Roberts DK, Thorne SE, Pearson C. Cancer Nurs 1993; 16:310-320.
American Academy of Hospice and Palliative Care (AAHPM) and Hospice and Palliative Nurses Association (HPNA) Measuring What Matters Project Top Ten Measures That Matter List
CMS Hospice Item Set
PEACE Hospice and Palliative Care Quality Measures Set Measure Algorithm:
| Related Topics |
Questions? Ask Question to Joint Commission staff
Copyright © 2018 by The Joint Commission.